Mohs micrographic surgery is a specialized technique used to treat complex skin cancers. It provides the highest rate of recovery, with a 99 percent cure rate for new skin cancers and a 95 percent cure rate for recurrent skin cancers, even when other treatments have failed.
Mohs Micrographic Surgery
Compared to standard procedures, Mohs surgery removes the smallest amount of healthy tissue, which minimizes scarring and preserves skin function and appearance. In addition, local anesthesia is used at the tumor site, eliminating the risks associated with general anesthesia.
Conditions Treated
Mohs micrographic surgery is used to treat complex basal cell and squamous cell cancers. In some instances, it used to treat less common tumors, including some superficial melanomas.
Skin cancers are considered complex in the following instances:
- The cancer is in an area where preserving healthy tissue is critical to maintaining a person's skin function and physical appearance, such as the eyelids, nose, ears, lips and hands.
- The cancer is in an area of high tumor recurrence, such as the ears, lips, nose, eyelids and temples.
- The cancer was not completely treated, or was previously treated and has recurred.
- The cancer is large.
- Edges of the cancer cannot be clearly defined.
- Scar tissue exists in the area of the cancer.
- Cancer is growing in an area previously treated by radiation therapy.
- The patient is immunosuppressed, such as those who have had an organ transplant, are HIV-positive or have chronic lymphocytic leukemia.
- The patient is at risk of multiple skin cancers because of conditions such as a genetic syndrome, basal cell nevus syndrome or xeroderma pigmentosa.
Preparation
Before surgery, a preoperative consultation with our team of experts may be scheduled to determine if Mohs surgery is the best treatment option. You may not need a preoperative consultation if you live far from UCSF Medical Center or if your referring doctor is familiar with Mohs surgery and can discuss it with you in detail.
When your appointment for surgery is scheduled, our nurse coordinator will contact you to discuss your medical history and any medications you are taking.
Mohs surgery is usually completed on an outpatient basis, meaning there's no overnight stay in the hospital. Please follow these instructions prior to surgery:
- Before your surgery, get a good night's rest and eat breakfast.
- Shower and shampoo your hair within 24 hours before your procedure to minimize bacterial growth on your skin and help prevent infection.
- Please arrive 30 minutes before your appointment to register. A map of UCSF Medical Center and travel instructions will be provided.
- Bring your insurance information and any insurance forms required for the procedure. Most insurance plans cover the cost, but please confirm with your insurer prior to surgery.
- Plan on being at UCSF for most of the day. Bring a book or magazine to read.
- Arrange for someone to drive you home after your surgery. If possible, ask a friend or family member to accompany you to UCSF.
Procedure
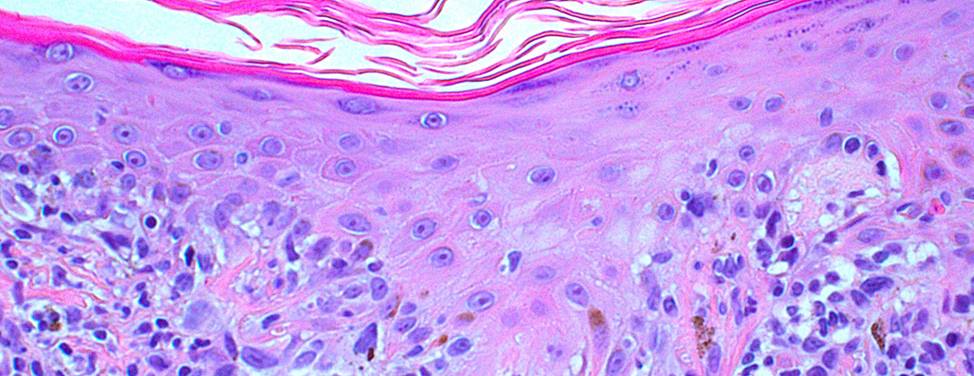
During Mohs surgery, tissue is surgically removed and its location precisely "mapped." The tissue is carefully examined microscopically by the surgeon on the same day of surgery. During this process, 100 percent of tissue margins around the tumor are evaluated to ensure that the tumor is completely removed before repairing the skin. As a result, Mohs surgery has the highest cure rate for complex skin cancers while minimizing the removal of normal tissue.
Standard surgical removal of skin cancer examines 1 percent of tissue margins around the tumor site and residual tumor tissue may be missed.
Step 1 — Anesthesia
Local anesthesia is used around the tumor site to numb the area. General anesthesia is not required for Mohs surgery.
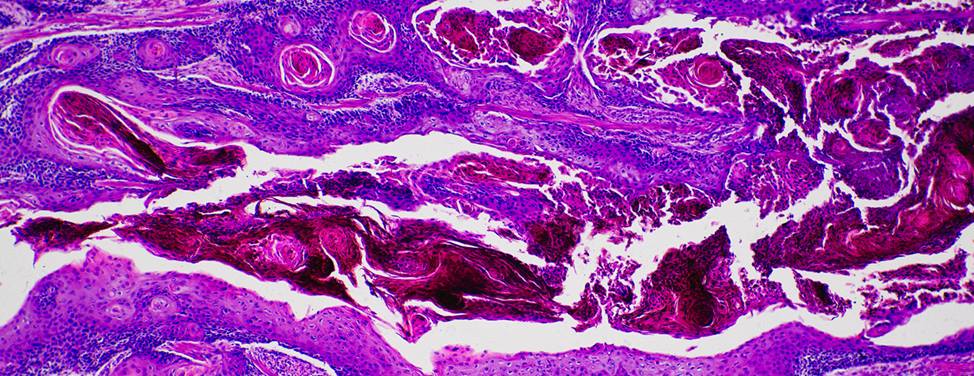
Step 2 — Remove the Tumor
After the skin is completely numb, the tumor is gently scraped with a curette, a semi-sharp, scoop-shaped instrument. This helps define the margin between tumor cells and healthy tissue. The first thin saucer-shaped "layer" of tissue is surgically removed by the surgeon. An electric needle may be used to stop bleeding. This process takes about 10 to 20 minutes.
Step 3 — Map the Tumor
After a layer of tissue has been removed, a "map" or drawing of the tissue and its orientation to "landmarks," such as the nose or cheek, is made as a guide to the precise location of the tumor. The tissue is labeled and color-coded to correlate with its position on the map.
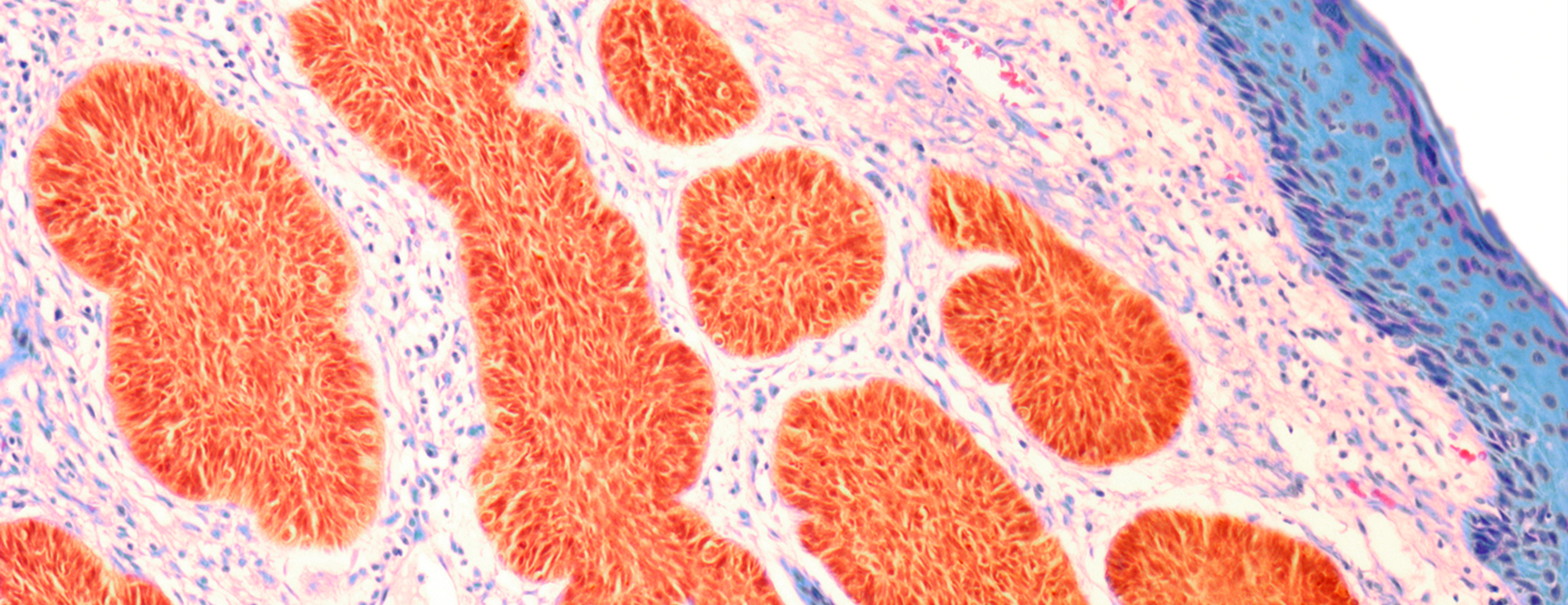
The tissue sections are processed and then examined by the surgeon to evaluate for evidence of remaining cancer cells. It takes about an hour to process, stain and examine a tissue section. During this processing period, your wound will be bandaged and you may leave the operating suite.
Step 4 — Ensure Cancer Cells Are Removed
If any section of the tissue shows cancer cells at the margin, the surgeon returns to that specific area, as indicated by the map, and removes another thin layer of tissue. The removed tissue is again mapped, color-coded, processed and examined. If microscopic analysis still shows evidence of disease, the process continues layer by layer until the cancer is completely removed.
Step 5 — Reconstruction
Mohs surgeons, who have completed fellowship training in the procedure, are experts in skin reconstruction to preserve normal skin function and physical appearance. The best method of repairing the wound after surgery is determined after the cancer is completely removed.
Stitches may be used to close the wound side-to-side, or a skin graft or a flap may be designed. Sometimes, a wound may be allowed to heal naturally. In rare cases, when Mohs surgery is extremely extensive or when removal of the tumor results in functional impairment, we may recommend that you visit one of our plastic surgeons for reconstruction.
Recovery
After your wound has healed, please return to your referring doctor for regular skin exams. We recommend six-month follow-up visits for two years and yearly thereafter if no additional cancers are detected. If any areas of your skin change in any way, fail to heal or cause concern, please let your doctor know immediately.
The surgery is generally well tolerated with few side effects but you may experience the following:
Pain
You will experience little discomfort after your surgery. Patients who do experience pain take Tylenol. Due to its potential to cause bleeding, please don't take aspirin or ibuprofen for pain control. In some cases, you may be prescribed a stronger pain medication.
Bleeding
A few patients experience some bleeding, which usually is controlled by the use of pressure. Take a gauze pad and apply constant pressure over the bleeding area for 15 minutes. Do not lift up or relieve the pressure during this period of time.
If bleeding persists after continued pressure for 15 minutes, repeat the pressure for another 15 minutes. If this fails, call your doctor. A doctor can be reached 24 hours a day by calling the answering service. This phone number will be given to you when you leave. Please don't drink alcohol the first night after surgery as this may stimulate bleeding.
Complications
Please notify us if you have an increase in your temperature, chills, increasing redness, swelling, drainage or escalating pain.
Minor complications that may occur after surgery include:
- A small red area surrounding your wound may appear. This is normal and does not necessarily indicate infection.
- Itching and redness around the wound, especially in areas where adhesive tape has been applied, are common. When this occurs, ask your pharmacist for a non-allergenic tape and let us know this occurred during your return visit.
- Swelling and bruising may occur, particularly when surgery is performed around the eyes. This usually subsides within four to five days after surgery and may be minimized by using an ice pack during the first 48 hours after surgery.
- At times, the area surrounding your operative site will be numb to the touch. This numbness may persist for several months and can be permanent. If this occurs, please tell your doctor at your follow-up visit.
Scarring can be minimized by the proper care of your wound. We will discuss wound care in detail with you.
Preventing Skin Cancer Recurrence
After having skin cancer, you are at a higher risk of developing it in the future. Skin damage from the sun cannot be reversed. Here are some precautions that can be taken to prevent further skin cancers:
- Apply SPF 30 or higher sunscreen at least 10 minutes before sun exposure.
- Reapply sunscreen frequently.
- Avoid excessive sun.
- Wear a wide-brimmed hat, long-sleeved shirt and other protective clothing.
- Ask your doctor to examine your skin every six months to check the surgical site as it is healing, and to look for the development of additional skin cancers.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.