Types of Pacemakers
There are many types of pacemakers, designed to treat a range of heart conditions. We use the full array at UCSF, and our heart team has expertise in implanting every kind. Here's help with understanding the types:
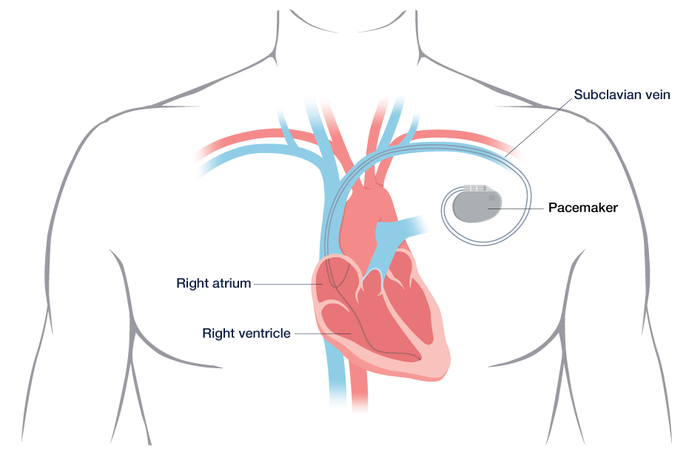
- A single-chamber pacemaker has a single lead that connects to the heart's lower right chamber (ventricle) or upper right chamber (atrium).
- A dual-chamber pacemaker has two leads that connect to both the upper and lower chambers on the heart's right side. This device helps control the timing of contractions between the chambers.
- A biventricular pacemaker has three leads, which connect to both chambers on the heart's right side plus the lower left ventricle. This type is used to regulate the heart's beating in some patients with advanced heart failure.
- A pacemaker may be combined with an implantable cardioverter-defibrillator (ICD), which can shock your heart back to a normal rhythm if it becomes dangerously fast. This device is used to prevent sudden death.
- A leadless pacemaker is implanted inside the heart through a minimally invasive procedure.
Your doctor will recommend the best type for you based on your symptoms and specific heart condition.
Evaluation
To determine whether a pacemaker is appropriate for your condition, you'll be checked for certain problems that may have damaged your heart's electrical system. These include:
- Age-related changes in the heart
- Coronary artery disease
- Heart attack
- Heart block (also called atrioventricular or AV block), a problem in the heart's electrical system that causes a slow heart rate
As part of your evaluation, you may have the following tests:
- Electrocardiogram (EKG) – a painless test that records the electrical activity of your heart and detects abnormal rhythms
- Echocardiogram – uses sound waves to create images of your heart, which can show blocked blood flow
- Stress test – a type of EKG that monitors your heart's ability to function during exercise
- Holter monitor – a portable EKG that you wear for 24 to 48 hours while it records your heart's activity
- Zio patch – a portable heart monitor that records your heart's rhythms for two weeks
Based on your test results and symptoms, your doctor will determine whether a pacemaker is right for you and, if so, which type. For instance, if the tests show you have a weak heart that doesn't contract in a coordinated way, you may be a candidate for a biventricular pacemaker.
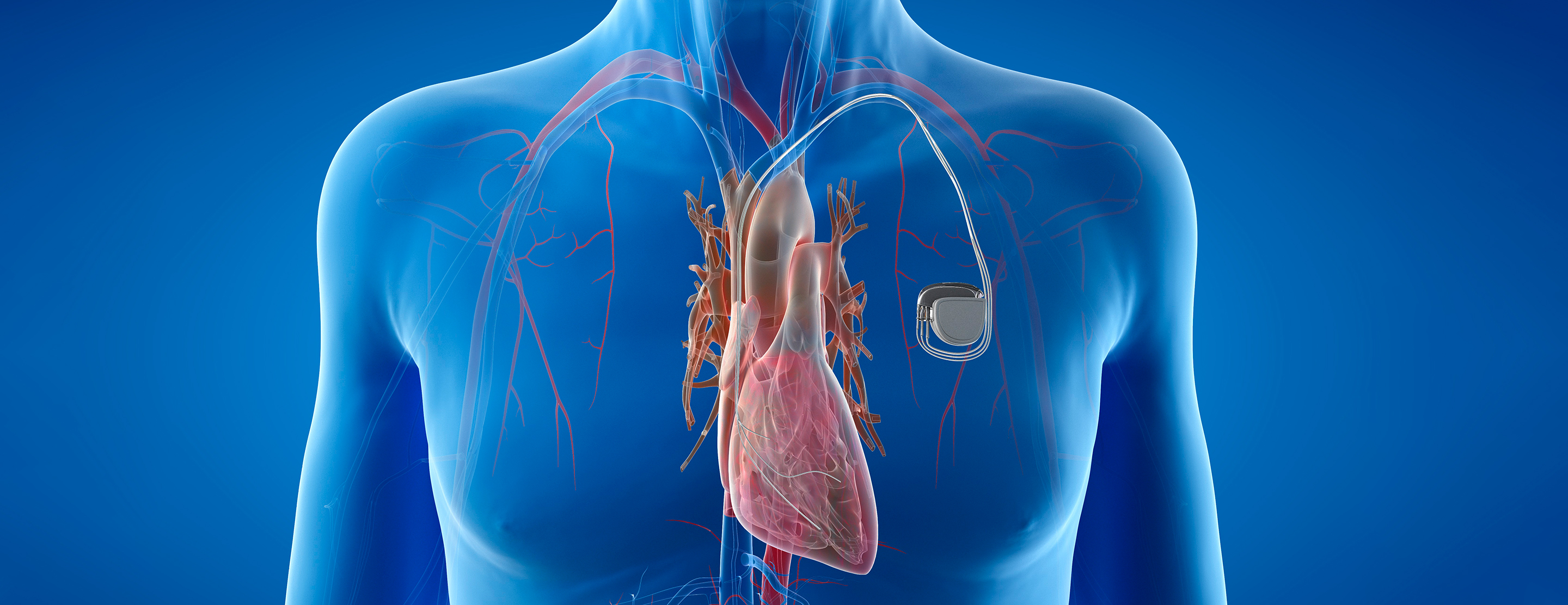
Procedure
The procedure to place a pacemaker depends on the type.
Pacemaker with leads – This requires a one- to three-hour surgery and general anesthesia. The surgeon makes a small incision just below your collarbone through which the lead is inserted into a nearby vein. Guided by X-ray images, the surgeon threads the lead to your heart and secures it in place with a tiny screw; the other end attaches to the pacemaker. Your doctor will then program the pulse generator and place it under the skin of your chest, near the collarbone. You may see a bump under the skin where the device is located.
Leadless pacemaker – This is implanted in a minimally invasive procedure, using a thin, flexible tube called a catheter to access the heart. After an injection to numb the area, a catheter containing the pacemaker is inserted into a blood vessel in your groin. The doctor threads the catheter through this vessel to the lower right chamber of your heart, then releases the pacemaker and attaches it to heart tissue. The catheter is then removed.
Recovery
After your procedure is finished, you'll be monitored in a post-op area for a brief period. Most patients spend the night in the hospital, but sometimes the procedure can be done safely on an outpatient basis, meaning you can go home the same day. Before discharge, your doctor will make sure the pacemaker is programmed properly for your needs.
Over the next month, you should avoid rigorous exercise and lifting anything heavier than 10 pounds. If you experience discomfort, you may need to take over-the-counter medications. Ask your doctors which pain relievers are safe for you.
You will be scheduled for a one-week checkup to make sure your incision looks OK. This may be in person or via video. About one month after the procedure, you will return for a follow-up visit with your doctor.
You will be monitored by our device clinic or your local doctor. We'll provide you with special equipment that allows you to hook up your pacemaker to a phone line for remote testing that looks at whether everything is functioning properly and detects any abnormal heart rhythms. The pacemaker can be reprogrammed as needed.
Risks
In general, the risks associated with a pacemaker are from the surgery to place it. Most are temporary, and life-threatening complications are rare. Risks include:
- allergic reaction to anesthesia
- bleeding
- bruising
- damaged nerves or blood vessels
- an infection at the incision site
- collapsed lung (very rare)
- punctured heart (very rare)
Electrical interference
Modern pacemakers are less sensitive to other electrical devices than older models, but certain appliances or machinery can still cause interference. For example, you should avoid:
- keeping a cell phone or MP3 player in a pocket over your pacemaker
- prolonged standing near certain appliances, such as microwave ovens
- prolonged exposure to a metal detector
- high-voltage transformers
Your doctor will provide more complete instructions on how to minimize your risks.