Ovulation Induction
Ovulation induction uses hormonal therapy to stimulate egg development and release, or ovulation. Historically, these drugs were designed to induce ovulation in women who did not ovulate on their own — typically women with irregular menstrual cycles. The goal was to produce a single, healthy egg.
The second use of ovulation induction was to increase the number of eggs reaching maturity in a single cycle, to increase chances for conception. The initial agents for this treatment — used first for in vitro fertilization (IVF) and only later for simpler treatments — were injectable medications. These agents carry an increased risk of multiple gestation, ovarian hyperstimulation, and increased cost and time commitment.
More recently, in the mid-90s, evidence developed to suggest there may be an advantage to treating even ovulatory women with fertility medications. These women with "unexplained infertility" may have subtle defects in ovulation, and medications may induce two to three eggs to mature, versus only one. This treatment therefore improves the quality and quantity of the ovulation, thus enhancing pregnancy rates.
In ovulatory women, ovulation induction is always combined with intrauterine insemination. Ovulation induction should progress only after a complete and thorough evaluation. All underlying hormonal disorders, such as thyroid dysfunction, should be treated before resorting to ovulation induction with fertility drugs.
The following common fertility drugs are used for ovulation induction.
Clomiphene Citrate (Seraphene and Clomid)
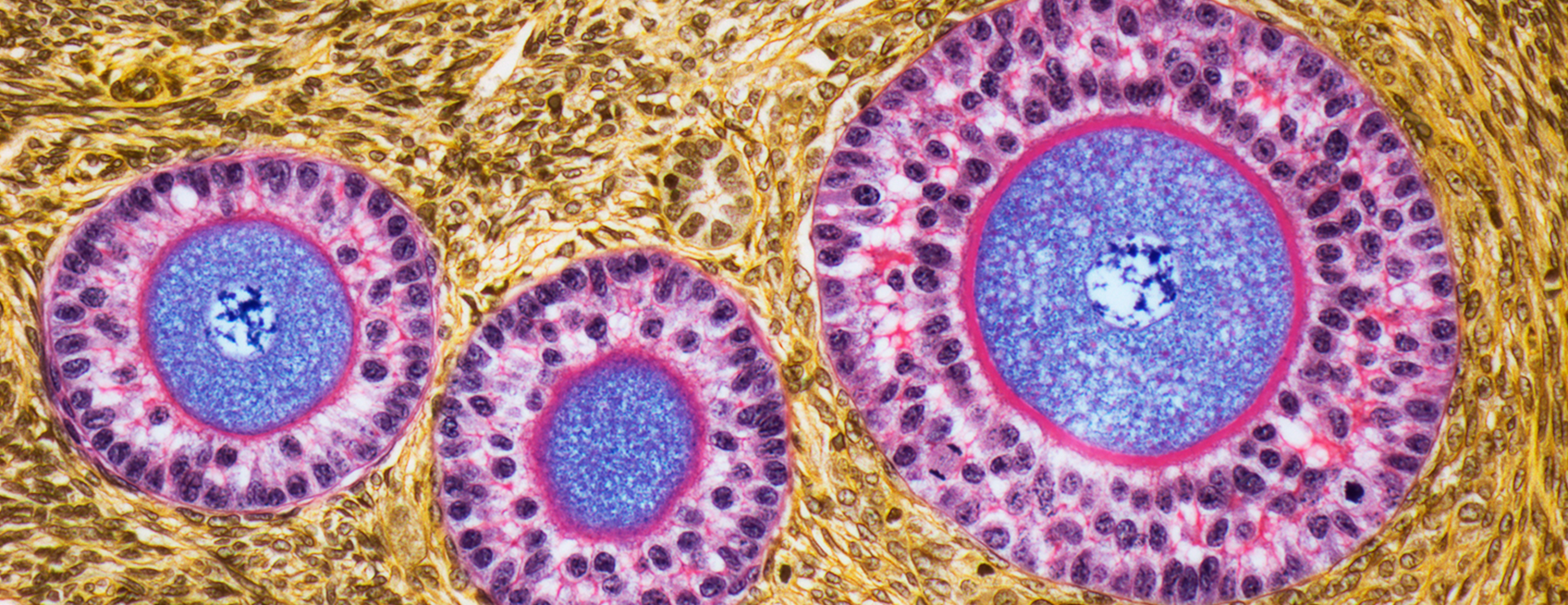
Clomiphene citrate is an oral medication that induces ovulation by blocking estrogen receptors. This artificial anti-estrogen effect makes your body believe that estrogen levels are low, which stimulates the production of more follicle stimulating hormone (FSH). Clomiphene citrate acts as a fertility agent in women by inducing superovulation — the release of multiple eggs in a given menstrual cycle.
Some form of monitoring is necessary while taking clomiphene citrate. This monitoring may include ultrasounds, blood estrogen levels, and urinary leutinizing hormone (LH) testing.
For unexplained infertility, clomiphene citrate is prescribed with intrauterine insemination (IUI). When used for ovulation induction in women who do not ovulate, IUI is not necessary.
Human Menopausal Gonadotropin (Pergonal, Humegon and Repronex)
Human menopausal gonadotropin (hMG) is a medication that is composed of follicle stimulating hormone (FSH) and leutinizing hormone (LH). It is used to stimulate egg development in women who do not ovulate spontaneously or who ovulate extremely irregularly, or to increase the number of eggs developed in a single cycle in women who already ovulate. Due to the variability in response from patient to patient, no fixed dosage regimen can be recommended. Each patient cycle must be individualized. However, it is generally thought to be a stronger superovulation agent than oral medications.
This fertility medication can be used with both intrauterine insemination (IUI) and in vitro fertilization (IVF).
Some form of monitoring of the ovarian response is necessary. A combination of blood estrogen measurement (E2) and ultrasound is the best approach at the present time. Monitoring minimizes the risk of complications.
Human menopausal gonadotropin is available only in injectable form. Self-administered injection techniques are taught in a special class given by the nursing staff at the UCSF Center for Reproductive Health.
Follicle Stimulating Hormone (Follistim/Gonal-F, Bravelle)
FSH medications are used to stimulate the recruitment and development of multiple eggs in women during an ovulation induction cycle. FSH products may be used alone or in combination with human menopausal gonadotropin (hMG) to induce superovulation.
Due to the variability in response from patient to patient, no fixed dosage regimen can be recommended. Each patient cycle must be individualized, with ultrasound exams and blood estrogen level tests to assess ovarian response. Monitoring minimizes the risk of complications.
FSH is available only in an injectable form. Self-administered injection techniques are taught in a special class given by the nursing staff at the UCSF Center for Reproductive Health.
Human Chorionic Gonadotropin (Profasi, Pregnyl, Ovidrel)
Human chorionic gonadotropin (hCG) is a natural hormone that helps with the final maturation of the eggs and triggers the ovaries to release the mature eggs (ovulation). It also stimulates the corpus luteum to secrete progesterone to prepare the lining of the uterus for implantation of the fertilized egg. Ovulation usually occurs about 36 hours after the hCG is given.
The drug is self-administered as an injection. Self-administered injection techniques are taught in a special class given by the nursing staff at the UCSF Center for Reproductive Health.
Leuprolide (Lupron) and Synthetic Gonadotropin (FSH/LH) Inhibitor
Lupron suppresses the brain's secretion of leutinizing hormone (LH) and follicle stimulating hormone (FSH). Therefore, it is used in preparation for cycles of treatment with ovulation induction drugs, such as exogenous hMG-LH/FSH and/or FSH. It improves the recruitment of follicles by preventing the recruitment of a dominant follicle for the next menstrual cycle. Lupron enables the ovaries to respond with the recruitment of multiple follicles since in most cases it's possible to override the selection of a single dominant follicle. It also prevents premature ovulation by preventing LH release.
To confirm the effectiveness of the Lupron treatment, an ultrasound is performed before the ovarian stimulation is begun and a blood estrogen level (E2) test may be required. Lupron also may be used to stimulate FSH if it is used early in the menstrual cycle. This property of the drug is helpful in patients expected to respond poorly.
Lupron is available in an injectable form. Self-administered injection techniques are taught in a special class given by the nursing staff at the UCSF Center for Reproductive Health.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.











