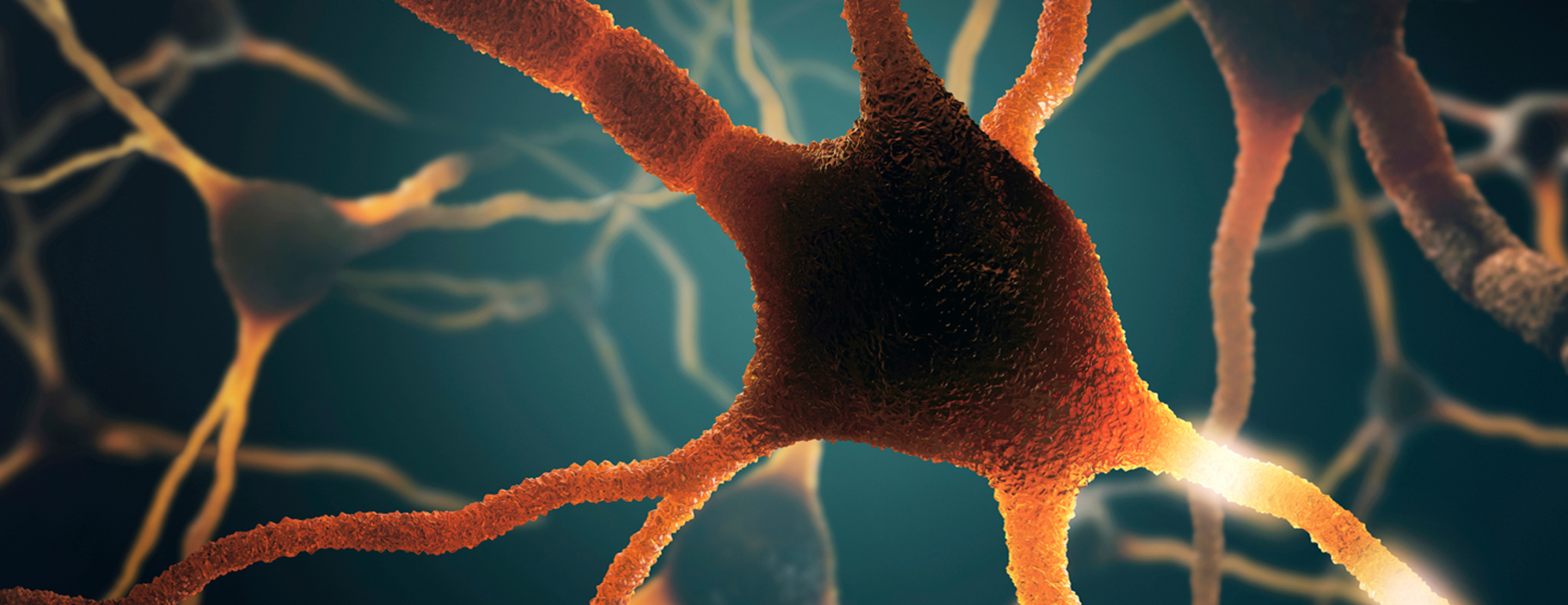
The sympathetic nerves are part of the autonomic nervous system, which controls the body's functions that we don't need to think about, such as blood pressure, digestion and heart rate. They also help us respond to "fight or flight" situations. Sympathetic nerves do not normally send pain messages to the brain but may become "switched on" for an unknown cause or due to a condition such as complex regional pain syndrome (CRPS), also known as reflex sympathetic dystrophy (RSD).
Nerve Blocks
A sympathetic nerve block involves injecting local anesthetic around a junction or "crossroads" where many nerves meet. The goal is to decrease or eliminate pain by reducing the pain signals sent to the brain.
Your doctor might suggest a nerve block if other treatments, such as anti-inflammatory medicines, rest and physiotherapy, were unsuccessful. Your doctor may also use nerve blocks as a diagnostic tool to determine whether your pain is actually coming from the sympathetic nervous system.
If you experience pain relief after a nerve block, your doctor may recommend additional nerve blocks or other forms of pain therapy to target the sympathetic nerves.
There are various sympathetic nerves located in different parts of the body, which may cause pain in the face, neck, arms, chest, lower back, legs and feet. The UCSF Pain Management Center offers the following types of nerve blocks:
- Sympathetic ganglion blockade
- Stellate ganglion blockade
- Lumbar sympathetic blockade
Preparation
Before your nerve block, your doctor will give you specific instructions for preparing for the procedure. These will depend on your condition, current state of health and any medications you are taking.
One week before the procedure:
Stop taking aspirin. If you take aspirin for your heart or blood vessels as prescribed by your doctor, please get written permission from your doctor to stop and bring that note to your procedure.
If you take Plavix (clopidogrel), you will need to stop taking it. Again, you will need verbal and written permission from your doctor to stop taking Plavix. Please bring the note to your procedure.
Three days before the procedure:
Stop taking herbal medicines and supplements, fish oil and Vitamin E.
24 hours before the procedure:
Stop taking anti-inflammatory medicines, such as Advil, ibuprofen, etodolac, indomethacin, naproxen, Aleve, Feldene, diclofenac, Mobic, and piroxicam. You do not need to stop taking Celebrex. If you are unsure about any of your medicines, ask your doctor. Call your doctor if you take blood thinners such as heparin or Coumadin (warfarin).
Day of the procedure:
Please arrange to have someone drive you home after the nerve block, as you will not be able to drive or operate machinery for at least 24 hours after the procedure.
You must be healthy on the day of your nerve block. You must:
- Be free of infection and not taking antibiotics
- Be free of cold or flu symptoms
- Be free of any rashes
- Not have a fever greater than 100.4° F
- Be free of any local infection or skin lesion
If you are feeling sick or have a cold, call us as soon as possible.
Procedure
During the procedure, you will lie on an X-ray table. You will have an intravenous (IV) line in your arm so that, if needed, we can give you medicine to help you relax.
The skin around the injection site will be cleaned and the area numbed with an anesthetic. The doctor will then use X-ray guidance to direct a needle to the targeted area and slowly inject anesthetic.
The procedure takes about 30 minutes.
Recovery
The degree of pain relief you experience will depend in part on whether your pain is actually caused by the sympathetic nerves. In the week after your procedure, it is helpful to keep a "pain diary" to share with your doctor.
Resume taking your regular medications, but please limit your use of pain medications the day of the procedure. This will make it easier to determine whether the nerve block was effective.
You may experience some mild pain around the injection site, which can be treated with ice. You may also experience a sensation of warmth in the targeted area for several hours after the procedure. This will resolve on its own.
On the side of the face that received an injection, you may experience symptoms such as smaller pupil size, drooping and lack of sweating. You may also have a hoarse voice. These symptoms resolve on their own and are not cause for worry.
On the day of the injection, you should avoid driving and all strenuous activities. On the day after the procedure, you may return to your regular daily activities. If your pain is improved, you may gradually resume regular exercise and more strenuous activities, increasing their frequency over one to two weeks to avoid recurrence of your pain.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.