FAQ: Lung Cancer Screening Program
What is the goal of a lung cancer screening using computed tomography (CT)?
The goal of any screening test is to prolong life. This is accomplished by detecting disease early, when it is potentially more treatable. For instance, some lung cancers found using CT screening are small and have not yet spread within the chest or to other areas of the body. Treatment is generally more effective at this stage. If screening is not performed, it is possible that a lung cancer would only be discovered after it has spread to other places in the body, at which point it is much more difficult to treat.
Who should be screened for lung cancer using CT?
Unlike many other screening programs, lung cancer screening CT is targeted to a specific group of patients. It is most useful for people who are at high risk for developing lung cancer, namely current or prior cigarette smokers. The length of time and number of cigarettes smoked affects whether a patient is a good candidate for CT screening. Most of the CT screening studies have been performed on patients who smoke 20 to 30 packs of cigarettes per year. A large research study, called The National Lung Screening Trial, evaluated patients whose smoking exceeded 30 packs per year. Pack-years are calculated by multiplying the average number of packs of cigarettes smoked each day times the total number of years smoked. If this number is equal to or greater than 30, you may benefit from a lung cancer screening CT. Patients with a family member who has been diagnosed with lung cancer may also benefit from CT screening.
What are the downsides of getting a screening CT?
There are two potential negative consequences of getting a screening CT: The first is radiation. This is addressed in the following section. The second potential downside is that the CT may prompt additional testing, and in some cases that testing is done to diagnose benign (not cancerous) growths. For instance, a suspicious pulmonary nodule may be surgically removed only to find out that it wasn’t a cancer. There are some similarities in the appearances of cancer and benign growths; thus a CT scan cannot give 100 percent assurance that an abnormal finding represents cancer. When a suspicious abnormality is seen, however, further testing is necessary with tests such as a PET scan, biopsy or surgery, which carry some side effects.
Should I be worried about the radiation I get from a CT?
Medical radiation has been a popular topic in the news recently and has raised concerns about the possibility of radiation-induced cancers. UCSF is very aware of this concern and has adopted many different techniques for reducing radiation from CT scans, including the development of low-dose protocols and the purchase of special software specifically designed for radiation reduction.
Each person is exposed to radiation in his or her daily life from the environment. The yearly dose that each person receives is approximately 3 millisieverts (mSv). In comparison, a standard chest CT imparts a dose of around 6 mSv (twice the yearly dose from the environment). It is estimated that the lifetime risk of developing a fatal cancer after receiving a dose of 10 mSv is 1 in 2000. Remember that, in general, one in four people will develop cancer in their lifetime. When considered in this context, the risk of developing a cancer from a CT scan only slightly increases a person’s overall risk from baseline.
Some people who get a screening CT will need one or more follow-up CTs for lung nodules. Small lung nodules have a low likelihood of representing cancer and are typically followed for a period of one to two years to ensure they are not growing. These additional CTs are performed using a low-dose technique that imparts a radiation dose of approximately 1/10th of a standard CT.
I have a lung nodule. Should I be worried?
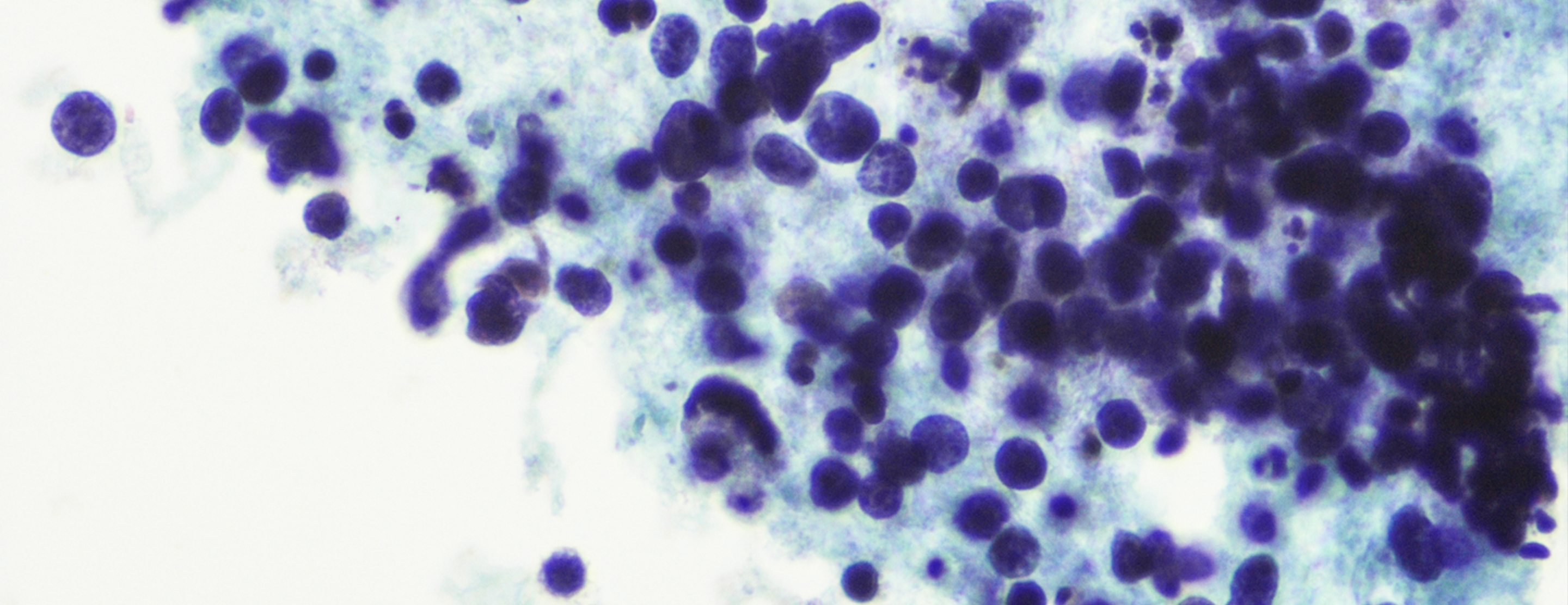
Lung nodules are very common, and the vast majority of them are benign (not cancerous). More than 50 percent of our patients can be expected to have a lung nodule found on CT, and more than 97 percent of these nodules will be benign. Any nodule has a possibility of representing cancer. The role of a CT scan is not only to detect nodules, but also to determine the likelihood that any nodule is benign or malignant based upon that nodule's features. Features of a nodule that is likely benign include small size, smooth borders and lack of growth over time. Nodules that are likely benign are typically followed with serial CT scans to make sure they are not growing. If they show no growth for a period of one to two years, they are considered to be benign and no further follow-up is required. If a nodule shows any suspicious features, some immediate action is generally warranted.
I have a suspicious lung nodule. What do I do next?
Patients with a lung nodule that demonstrates suspicious features on a CT scan should be referred to a specialist in either pulmonary medicine or thoracic surgery to manage the work-up of that nodule. Patients in the Lung Screening Program can discuss the results of their CT scan with one of the program’s pulmonary medicine specialists. Suspicious features of a nodule include large size, irregular or spiculated borders and growth over time. The next step in the work-up of that nodule depends upon multiple factors. Options include PET scanning, CT-guided lung biopsy, bronchoscopy and surgery. The test that is used will depend on the appearance of your CT scan, smoking history, age, symptoms and presence of other diseases.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.






