Cytology exam of pleural fluid
Definition
A
Alternative Names
Pleural fluid cytology; Lung cancer - pleural fluid
How the Test is Performed
A sample of fluid from the pleural space is needed. The sample is taken using a procedure called
The procedure is done in the following way:
- You sit on a bed or on the edge of a chair or bed. Your head and arms rest on a table.
- A small area of skin on your back is cleaned. Numbing medicine (local anesthetic) is injected in this area.
- The doctor inserts a needle through the skin and muscles of the chest wall into the pleural space.
- Fluid is collected.
- The needle is removed. A bandage is placed on the skin.
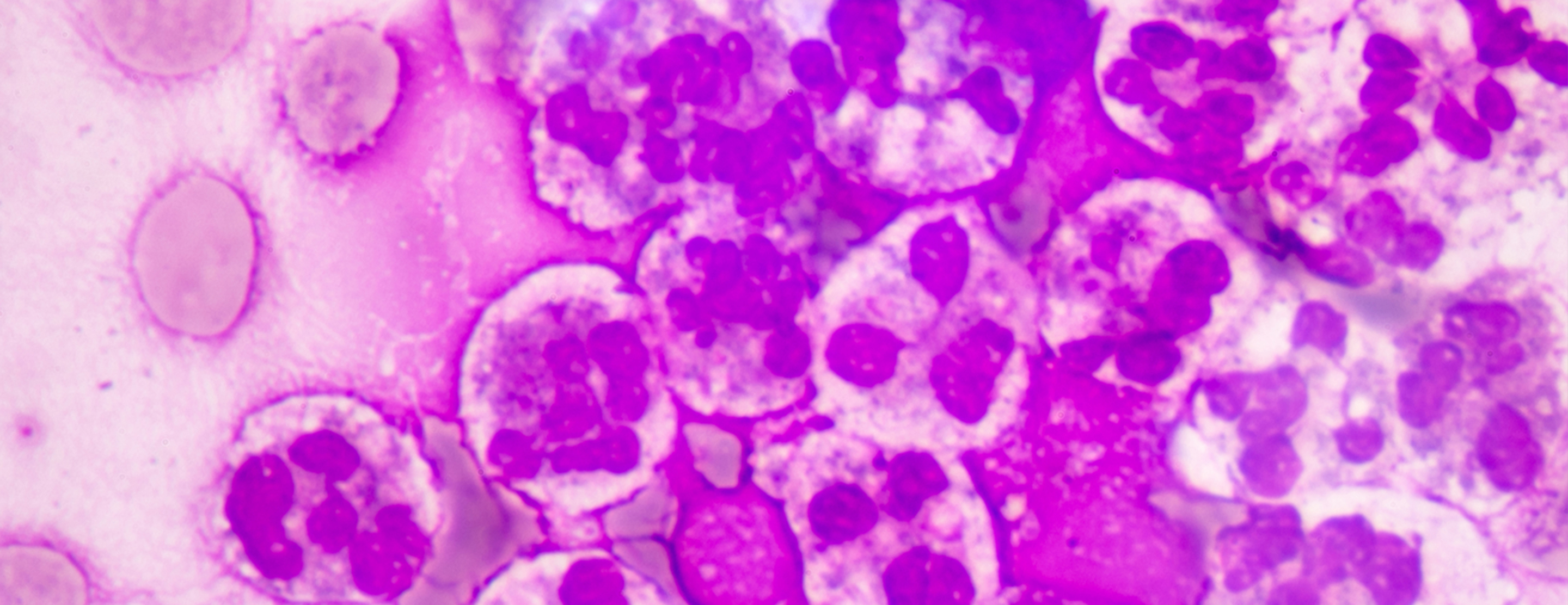
The fluid sample is sent to a laboratory. There, it is examined under the microscope to determine what the cells look like and whether they are abnormal.
How to Prepare for the Test
No special preparation is needed before the test. A chest x-ray will likely be done before and after the test.
DO NOT cough, breathe deeply, or move during the test to avoid injury to the lung.
How the Test will Feel
You will feel stinging when the local anesthetic is injected. You may feel pain or pressure when the needle is inserted into the pleural space.
Tell your health care provider if you feel short of breath or have chest pain.
Why the Test is Performed
A cytology exam is used to look for cancer and precancerous cells. It may also be done for other conditions, such as identifying
Your doctor may order this test if you have signs of fluid buildup in the pleural space. This condition is called
Normal Results
Normal cells are seen.
What Abnormal Results Mean
In an abnormal test, there are cancerous (malignant) cells. This may mean there is a cancerous
Breast cancer Lymphoma Lung cancer - Ovarian cancer
- Stomach cancer
Risks
Risks are related to thoracentesis and may include:
- Bleeding
- Infection
- Collapse of the lung (
pneumothorax ) - Difficulty breathing
References
Blok BK. Thoracentesis. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges' Clinical Procedures in Emergency Medicine and Acute Care. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 9.
Cibas ES. Pleural, pericardial, and peritoneal fluids. In: Cibas ES, Ducatman BS, eds. Cytology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 4.
Chernecky CC, Berger BJ. Thoracentesis - diagnostic. In: Chernecky CC, Berger BJ, eds. Laboratory Tests and Diagnostic Procedures. 6th ed. St Louis, MO: Elsevier Saunders; 2013:1052-1135.
Review Date: 07/20/2018
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. Copyright ©2019 A.D.A.M., Inc., as modified by University of California San Francisco. Any duplication or distribution of the information contained herein is strictly prohibited.
Information developed by A.D.A.M., Inc. regarding tests and test results may not directly correspond with information provided by UCSF Health. Please discuss with your doctor any questions or concerns you may have.





