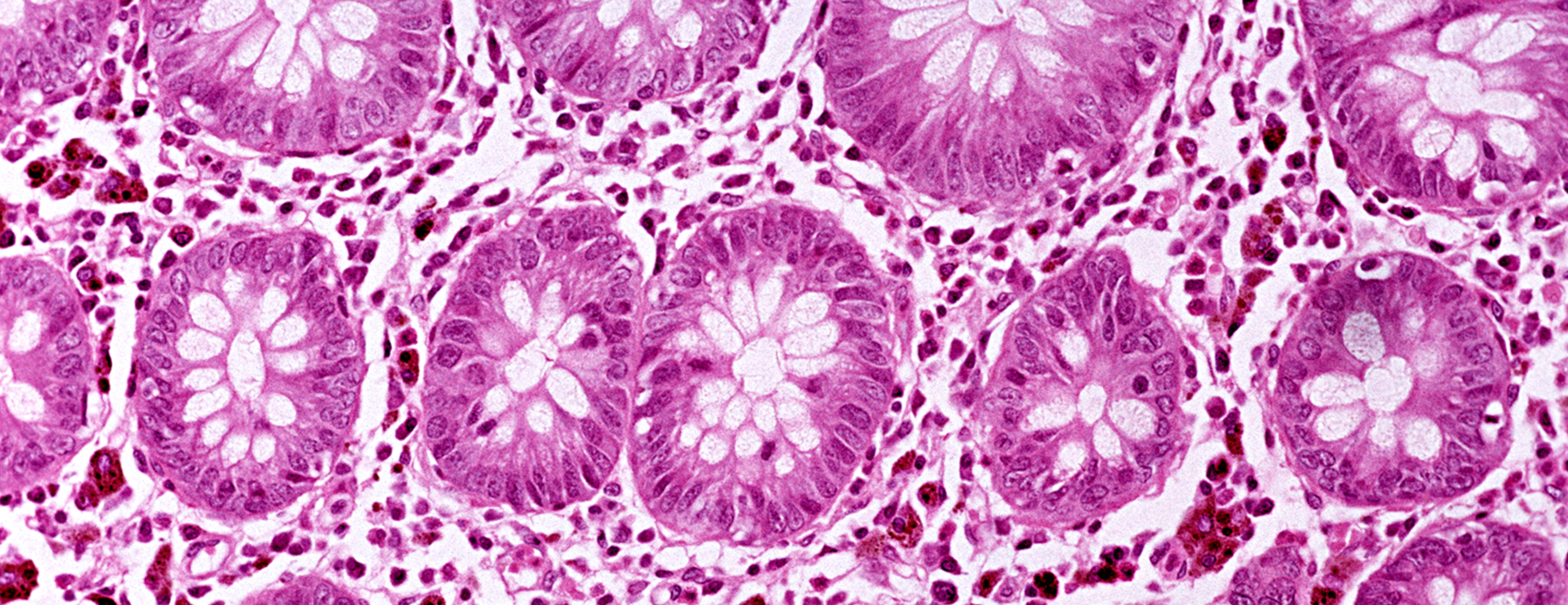
Culture - colonic tissue
Definition
A colonic tissue culture is a lab test to check for the cause of disease. The sample of tissue for the test is taken from the large intestine. The cause may be bacteria, fungi, or viruses.
Alternative Names
Colonic tissue culture
How the Test is Performed
The health care provider removes a piece of tissue from your large intestine. This is done during a
- The sample is sent to a lab.
- It is placed in a special dish that contains a gel. Bacteria and other organisms can grow in this gel. The dish is then stored at a certain temperature.
- The lab team checks the sample daily. They check to see if bacteria, viruses, or fungi have grown.
If certain germs grow, more tests will be done to identify them. This helps decide the best treatment.
How to Prepare for the Test
There is no specific preparation needed for a culture.
How the Test will Feel
Once the sample is taken, the culture does not involve you. Therefore, there is no pain.
Why the Test is Performed
Your provider may order this test if you have signs or symptoms of a large intestine infection. A culture is often done when other tests such as a
Normal Results
A normal result means that no disease-causing organisms have grown in the lab dish.
Some "healthy" bacteria, called bowel flora, are normally found in the gut. The growth of such bacteria during this test does not mean there is an infection.
Normal value ranges may vary slightly among different laboratories. Talk to your provider about your test results.
What Abnormal Results Mean
An abnormal result means that disease-causing organisms have grown in the lab dish. These organisms may include:
- Clostridium difficile bacteria
- Cytomegalovirus
- Mycobacterium tuberculosis bacteria
Salmonella bacteria - Shigella bacteria
These organisms may lead to
Risks
There are no risks in a colonic tissue culture.
References
DuPont HL. Approach to the patient with suspected enteric infection. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 283.
Hall GS, Woods GL. Medical bacteriology. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. Philadelphia, PA: Elsevier; 2017:chap 58.
Haines CF, Sears CL. Infectious enteritis and proctocolitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 10th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 110.
Semrad CE. Approach to the patient with diarrhea and malabsorption. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 140.
Siddiqi HA, Salwen MJ, Shaikh MF, Bowne WB. Laboratory diagnosis of gastrointestinal and pancreatic disorders. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. Philadelphia, PA: Elsevier; 2017:chap 22.
Review Date: 04/11/2018
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. Copyright ©2019 A.D.A.M., Inc., as modified by University of California San Francisco. Any duplication or distribution of the information contained herein is strictly prohibited.
Information developed by A.D.A.M., Inc. regarding tests and test results may not directly correspond with information provided by UCSF Health. Please discuss with your doctor any questions or concerns you may have.





