Acute Lymphoblastic Leukemia
Treatments
The treatment of acute lymphoblastic leukemia (ALL) varies according to one's age, general condition at diagnosis and the results of the cytogenetic testing. Standard therapy for ALL has changed very little in the last 15 years or so, as the current strategy has been very effective at curing adults. The goal of treatment is a cure. Treatment can be divided into four phases:
- First phase — induction chemotherapy
- Second phase — consolidation chemotherapy
- Third phase — maintenance chemotherapy
- Fourth phase — central nervous system (CNS) prophylaxis
The first two phases use intensive chemotherapy medications designed to kill the leukemia cells that grow quickly. Complete therapy for ALL typically continues for two to three years.
Complete remission — a cure — is achieved in approximately 90 percent of patients, with 25 percent to 40 percent enjoying long-term survival. About 5 percent of patients die of treatment-related complications during their initial therapy, and another 5 percent never achieve an initial remission.
Chemotherapy
Treatment of ALL is usually urgent and needs to be given within days, and sometimes the same day, as the diagnosis is made. The first phase of treatment, called induction chemotherapy, requires that patients remain in the hospital for approximately four weeks.
Induction Chemotherapy
The most common drugs used for induction treatment of ALL are daunorubicin, vincristine, prednisone, asparaginase and sometimes cyclophosphamide. Intensive supportive care accompanies the chemotherapy, including transfusion of red blood cells and platelets. Antibiotics are needed both preventatively and as treatment for both bacterial and fungal infections. The agent G-CSF (Neupogen) can be useful in rapidly reestablishing a normal white blood count. Although the likelihood of mouth sores and disruption of the intestinal tract is rare, complete but temporary hair loss does occur.
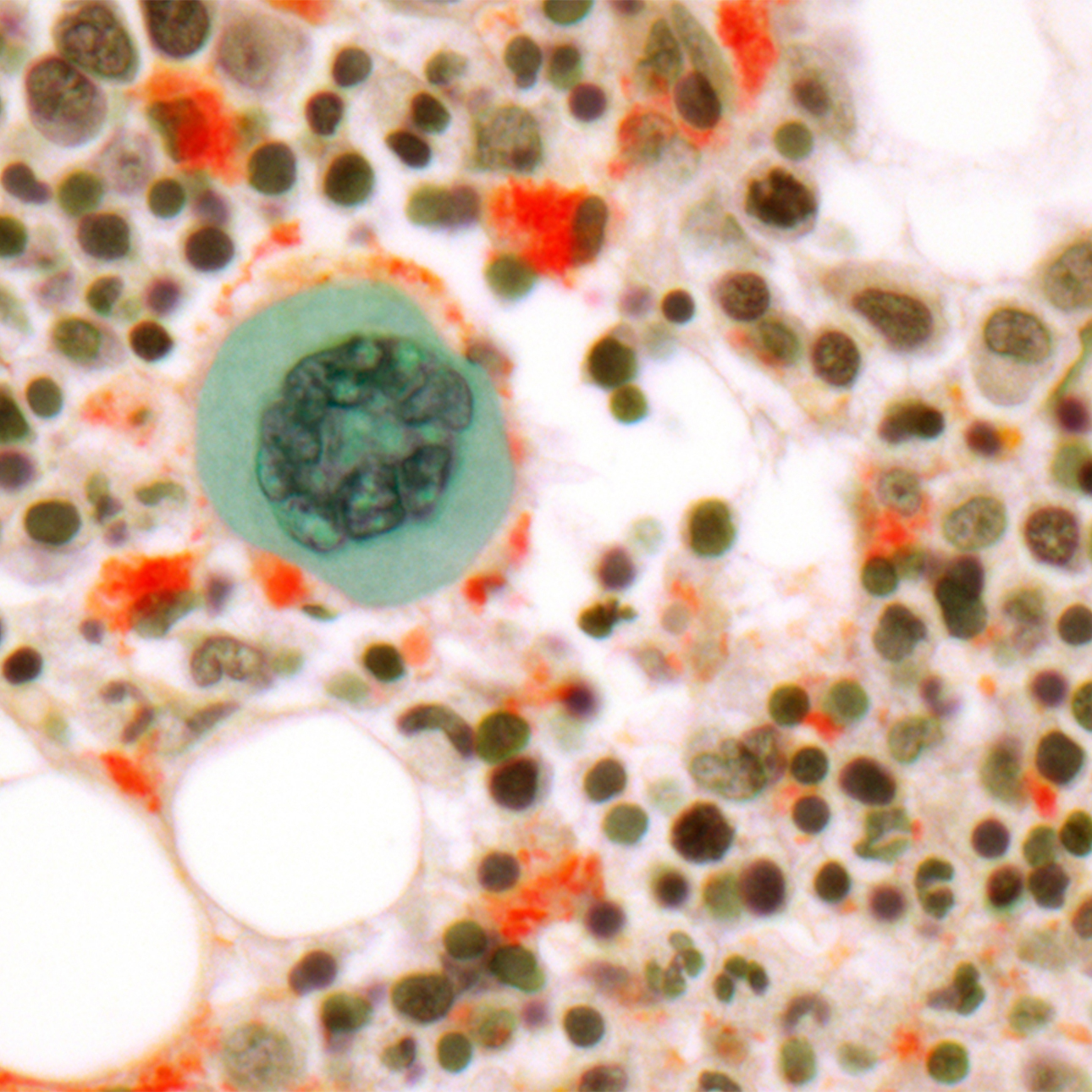
Once blood counts have returned to normal, a repeat bone marrow biopsy is performed to determine whether the patient has entered complete remission. A complete remission is achieved when the blood and bone marrow show no evidence of persistent leukemia and blood counts have returned to normal.
Consolidation Chemotherapy
Consolidation chemotherapy typically includes multiple cycles of intensive chemotherapy given over a six- to nine-month period. Frequent hospitalizations are required and intensive supportive care is still needed, including red blood cell and platelet transfusions. Stem cell transplantation is not typically performed to treat ALL unless abnormal cytogenetics are present.
Chemotherapy agents used during consolidation include the same agents used during induction, as well as Ara-C, etoposide, methotrexate and 6-mercaptopurine.
Maintenance Chemotherapy
Once patients have completed intensive chemotherapy, they need to take oral chemotherapy pills for an additional 18 to 24 months. These oral chemotherapy pills — typically methotrexate and 6-mercaptopurine — are usually well-tolerated with only minimal side effects. Patients need to have their blood tests checked once a month while taking chemotherapy pills. Most patients with ALL can return to work during maintenance therapy.
Central Nervous System (CNS) Prophylaxis
ALL frequently can recur in the spinal fluid, the fluid that bathes the spinal column and brain. To prevent relapse at this location, chemotherapy must be injected directly into the fluid that bathes the spinal column. This is done by inserting a needle between the vertebrae of the lower back — called a spinal tap or lumbar puncture — and infusing chemotherapy directly into the clear spinal fluid. This is called intrathecal chemotherapy.
Patients are routinely given six or more injections of intrathecal chemotherapy to prevent recurrence of ALL. More injections may be necessary if leukemia cells are detected in the spinal fluid.
Most people complete intrathecal therapy within two to four months of starting their treatment. Headaches and nausea are occasional side effects.
Adjunctive therapies
Up to one-quarter of adults with ALL have the "Philadelphia chromosome" in their leukemia cells, which confers a poor prognosis. There are several FDA-approved drugs available to such patients, including imatinib (Gleevec) and dasatinib (Sprycel). Patients begin taking them during induction chemotherapy and continue indefinitely. Such ALL patients are typically given an allogeneic bone marrow transplant as their best chance of a cure.
ALL patients are prone to viral infections and to a pneumonia called pneumocystis during their treatment. Preventative antibiotics, such as acyclovir and Septra or Bactrim, are given during ALL therapy.
Stem cell transplantation
Stem cell transplantation, also called blood or marrow transplantation (BMT), is performed only in patients who have abnormal cytogenetics, chromosome testing or other high-risk ALL features. Cytogenetics is the most important component of deciding whether or not a person should have a bone marrow transplant for ALL. Patients with the Philadelphia chromosome or with the translocation involving chromosomes 4 and 11, should go on to BMT.
At UCSF Medical Center, allogeneic transplantation — which uses stem cells or bone marrow from a matched brother or sister — is preferred and considered the standard therapy for ALL. Young patients with very high-risk ALL who need an allogeneic transplant but lack a matched sibling donor are sometimes appropriately treated with allogeneic transplant using a matched unrelated donor identified though the National Marrow Donor Program (NMDP).
At UCSF we also offer autologous transplantation — which uses cells collected from the patient's own blood after they have achieved complete remission — for patients with high-risk ALL who lack compatible donors.
The autologous stem cell transplantation protocol is an investigational therapy. Following successful induction therapy, patients with high-risk ALL are given one cycle of intensive consolidation chemotherapy. When the blood counts begin to return to normal after consolidation therapy, stem cells are collected from the blood using a technique called apheresis. A large IV catheter called a Quentin catheter is inserted into one of the large veins in the neck. This catheter is connected to an apheresis machine, which acts as a centrifuge that separates the blood into individual components, allowing the collection of only the white blood cells. All the other cells, including red blood cells and platelets, are given back to the patient.
Each apheresis procedure takes four hours, and two to three procedures are usually necessary to collect enough stem cells. After completing radiation and chemotherapy, the autologous stem cells are thawed out and re-infused through the vein to restart blood production.
High-dose therapy in the ALL protocol includes both radiation therapy and chemotherapy. The hospitalization for the high-dose radiation, chemotherapy and re-infusion of autologous peripheral blood stem cells lasts approximately four weeks. The side effects are severe and aggressive supportive care measures are needed.
Investigational therapies
UCSF is dedicated to improving outcomes of ALL patients through the use of investigational therapies and clinical research trials. A recent trial will substitute a long-acting drug, peg-asparaginase, for the regular asparaginase, in the standard UCSF ALL regimen. Peg-asparaginase has fewer side effects and perhaps better remission rates than regular asparaginase. We are also exploring using Ara-C packaged in balls of fat called liposomes (Depocyte) as intrathecal chemotherapy to prevent CNS relapse of ALL.
In addition, we currently have experimental medications to treat patients with rare types of the Philadelphia chromosome that don't respond to imatinib or dasatinib.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Treatments we specialize in
-
Allogeneic Transplant
In a procedure similar to a simple blood transfusion, the patient receives bone marrow or stem cells from a tissue-matched donor.
Learn more -

Autologous Transplant
Stem cells collected from the blood before chemotherapy or radiation are returned to the patient's body using a process similar to a blood transfusion.
Learn more




















