Complete Heart Block
Treatments
Depending on the type and severity of your arrhythmia, and the results of various tests including the electrophysiology study, there are several treatment options. You and your doctor will decide which one is right for you.
Medications
Certain anti-arrhythmic drugs change the electrical signals in the heart and help prevent abnormal sites from starting irregular or rapid heart rhythms.
Follow-up Electrophysiology Study
To make sure the medication is working properly after two or more days in the hospital, you may be brought back to the laboratory for a follow-up study. Our goal is to find the drug that works best for you.
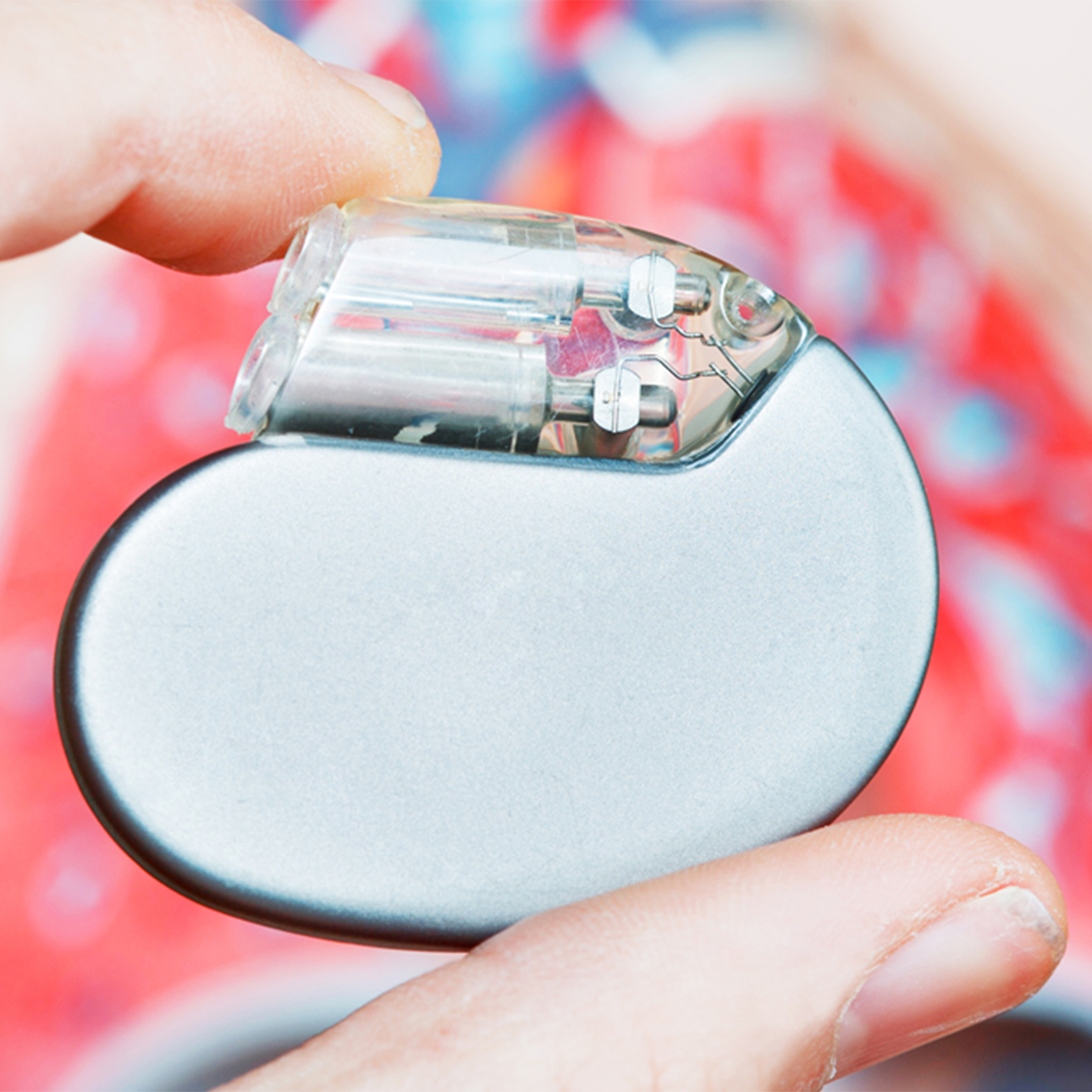
Implantable Device (Pacemaker)
All implantable devices or pacemakers work on "demand" and are used to treat slow heart rhythms. They are small devices that are implanted beneath the skin below the collarbone and connected to a pace wire(s) positioned inside the heart via a vein; this delivers a small electrical impulse to stimulate the heart to beat when it is going too slow.
Catheter Ablation
A technique pioneered at UCSF, radiofrequency catheter ablation destroys or disrupts parts of the electrical pathways causing the arrhythmias, providing relief for patients who may not have responded well to medications, or who would rather not or can't take medications.
Catheter ablation involves threading a tiny metal-tipped wire catheter through a vein or artery in the leg and into the heart. Fluoroscopy, which allows cardiologists to view on a monitor the catheter moving through the vessel, provides a road map. Other catheters, usually inserted through the neck, contain electrical sensors to help find the area causing the short-circuits. The metal-tipped catheter is then maneuvered to each problem site and radiofrequency waves — the same energy used for radio and television transmission — gently burn away each unwanted strand of tissue. When catheter ablation was first tried, direct current shocks were used, but researchers later developed the use of radiofrequency waves — a more precise form of energy. With radiofrequency catheter ablation, patients usually leave the hospital in one day, compared to open heart surgery, which requires a week stay and months of recovery.
For conditions like Wolff-Parkinson-White syndrome, in which a hair-thin strand of tissue creates an extra electrical pathway between the upper and lower chambers of the heart, radiofrequency ablation offers a cure. It has become the treatment of choice for patients with that disorder who don't respond well to drug therapy or who have a propensity for rapid heart rates.
Even in arrythmias that can be controlled with drugs, the procedure has been shown to be cost effective because it eliminates medication failures that require hospitalization. It also is an attractive option for elderly patients who are prone to suffer side effects from drug therapy and women of childbearing age who can't take medications because of potential health risk to the fetus.
While studies have shown that catheter ablation is more cost effective than drug therapy or surgery, patients who undergo the procedure also experience remarkable improvement in quality of life. A recent study of nearly 400 ablation patients with dangerously rapid heart rates — nearly a third of whom were considered candidates for open heart surgery — found that one month after the procedure 98 percent required no medication and 95 percent reported that their overall health had markedly improved. The UCSF study also found improvement in the patients' ability to work, exercise and take on physical activities.
Internal Cardioversion
Internal cardioversion for conversion of atrial fibrillation and atrial flutter to a normal sinus rhythm was developed here at UCSF Medical Center in 1991. Internal cardioversion is low energy electrical shock (1 to 10 joules) delivered internally in the heart through two catheters inserted in a vein in the groin and a small electrode pad applied to the chest. This procedure is performed in the electrophysiology lab by our electrophysiologist.
During the internal cardioversion, short-acting sedatives are given to make the patient sleepy. Currently, atrial flutter is successfully "cured" by radiofrequency catheter ablation; but treatment to restore atrial fibrillation to sinus rhythm has been the traditional use of medications and external cardioversion. External cardioversion is delivery of high energy shocks of 50 to 300 joules through two defibrillator pads attached to the chest. In some cases, external cardioversion has failed because the electrical current has to first travel through chest muscle and skeletal structures before reaching the heart. Internal cardioversion has been performed when medications and external cardioversion have failed to restore a patient's rhythm back to a normal sinus rhythm.
UCSF's success rate of converting a patient from atrial fibrillation to normal sinus rhythm with internal cardioversion has been 95 percent. The less time a patient is in atrial fibrillation, the easier it is to cardiovert back to a normal rhythm, but even patients with long-standing chronic atrial fibrillation can be converted successfully to a normal rhythm through internal cardioversion. With internal cardioversion, our electrophysiology team was successful in converting a patient who had been in chronic atrial fibrillation for eight years.
Implantable Cardioverter Defibrillator
An implantable cardioverter defibrillator is a device for people who are prone to life-threatening rapid heart rhythms. It is slightly larger than a pacemaker and usually is implanted beneath the skin below the collarbone. It is connected to a defibrillation/pace wire(s) positioned inside the heart via a vein. It has the capability of delivering an electric shock to the heart when it determines the heart rate is too fast. It also is capable of pacing or stimulating the heart when it is going too slow.
Biventricular Pace Maker
The U.S. Food and Drug Administration (FDA) recently approved the first of a new type of pacemaker that paces both ventricles of the heart to coordinate their contractions and improve their pumping ability. According to the test results presented to the FDA, cardiac resynchronization therapy (CRT):
- Increases the amount of daily activities patient can perform without the symptoms of heart failure
- Extends the exercise capacity of heart failure patients as measured by the distance they can walk in 6 minutes
- Improves the overall quality of life as judged by standard measurements
- Promotes changes in heart anatomy to improve cardiac function
- Reduces the number of days patients spend in the hospital and the total number of hospitalizations
CRT devices work by pacing both the left and right ventricles simultaneously, which results in resynchronizing the muscle contractions and improving the efficiency of the weakened heart. In the normal heart, the electrical conduction system delivers electrical impulses to the left ventricle in a highly organized pattern of contractions that pump blood out of the ventricle very efficiently. In systolic heart failure caused by an enlarged heart (dilated cardiomyopathy), this electrical coordination is lost. Uncoordinated heart muscle function leads to inefficient ejection of blood from the ventricles.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Treatments we specialize in
-

Catheter Ablation
The minimally invasive technique has become the treatment of choice for arrhythmia patients who do not respond well to medication.
Learn more -
Implantable Cardioverter Defibrillator
A small implanted device helps regulate the heart rate in patients who experience very fast heart rhythms.
Learn more -

Pacemaker
Millions of people now rely on these tiny electronic devices to keep their hearts beating steadily.
Learn more










