Trigeminal Neuralgia
Treatments
Medication is always the first line of treatment for trigeminal neuralgia. Patients who continue to experience pain despite the best medical management will be evaluated for surgery.
Medical Treatments for Trigeminal Neuralgia
The medicines doctors typically prescribe to treat trigeminal neuralgia were originally developed to treat epilepsy. However, this class of medications, called anti-convulsants, has been found to be quite effective in treating nerve pain, including trigeminal neuralgia, when taken on an ongoing basis.
The anti-convulsant drug most commonly prescribed for trigeminal neuralgia is carbamazepine (Tegretol), which can provide at least partial pain relief for up to 80 to 90 percent of patients. Other anti-convulsants prescribed frequently for trigeminal neuralgia include:
- Phenytoin (Dilantin)
- Gabapentin (Neurontin)
- Lamotrigine (Lamictal)
- Oxcarbazepine (Trileptal)
- Topiramate (Topamax)
The muscle relaxant baclofen (Lioresal) may also be prescribed, either alone or in combination with other drugs.
Side Effects
The most common side effects from these medicines are dizziness, drowsiness, forgetfulness, unsteadiness and nausea. In addition, these drugs do not always remain effective over time, requiring higher and higher doses or a greater number of medications taken together. Some patients experience side effects serious enough to warrant discontinuing the medication.
Surgical Treatments for Trigeminal Neuralgia
Trigeminal neuralgia surgery is reserved for people who still experience debilitating pain despite the best attempts to manage their condition with medication. Surgery for trigeminal neuralgia is rarely attempted on patients with non-trigeminal neuralgia face pain or on atypical trigeminal neuralgia, since operations for these conditions have much lower success rates and, in many cases, can make the pain worse and/or cause additional medical problems.
Microvascular Decompression
Microvascular decompression (MVD), also known as the Jannetta procedure, is the most common surgical procedure for treating trigeminal neuralgia. In the procedure, the surgeon makes a small incision behind the ear and drills a small hole in the skull. Using microscopic visualization, the trigeminal nerve is exposed. In most cases, there is a blood vessel — typically an artery, but sometimes a vein — compressing the trigeminal nerve. By moving this blood vessel away from the nerve and interposing a padding made of Teflon felt, the pain is nearly always relieved.
While MVD is considered to be the most invasive surgery for trigeminal neuralgia, it is also the best procedure for fixing the underlying problem: vascular compression. MVD also causes the least damage to the trigeminal nerve and provides, on average, the longest pain-free periods and the best chance for the patient to be permanently off medication. MVD has a long-term success rate of approximately 80 percent as a stand-alone treatment. The procedure requires an average hospital stay of two to three days, and four to six weeks to return to normal daily activities.
MVD is a major surgery, and includes craniotomy, cutting a small hole in the skull. Typical surgical risks for any open-skull neurosurgical procedure include infection, excessive bleeding, spinal fluid leakage and risks of anesthesia. Rare neurological injury can include damage to hearing, vascular injury (stroke) and, very rarely, death.
Gamma Knife Radiosurgery
Gamma Knife is the least invasive surgical option for trigeminal neuralgia. In fact, it is technically not surgery at all. The Gamma Knife is a device that delivers precise, controlled beams of radiation to targets inside the skull, including the brain and associated nerves. For trigeminal neuralgia treatment, the radiation beams are aimed at the trigeminal nerve where it enters the brainstem.
Gamma Knife treatment does not target the root cause of trigeminal neuralgia, but instead damages the trigeminal nerve to stop the transmission of pain signals. The procedure requires little or no anesthesia, and is performed on an outpatient basis.
This procedure provides significant pain control or reduction in approximately 80 percent or more of patients, but response is usually slower than for other treatments. Patients usually begin to respond to the treatment within four to 12 weeks post-treatment, but some patients require as much as six to 12 months for the full response. Most patients remain on full doses of their trigeminal neuralgia medication for at least three to six months after treatment. Typically, we do not start to taper the patient's medications until pain relief has been achieved.
Side effects may include tingling or numbness in the face, seen in up to 20 to 30 percent of patients. If they do occur, these symptoms do not typically appear until six to 24 months following treatment. The resulting numbness (sometimes referred to as paresthesias or dysesthesias) can range in intensity from mild to severe and may affect the entire side of the face.
Radiofrequency Lesioning
Radiofrequency lesioning, also called radiofrequency rhizotomy, is a good option for severe pain in high-risk patients, such as patients with an additional illness that would make an open surgical procedure too dangerous. It is also a good option for patients with multiple sclerosis (MS), whose trigeminal neuralgia often is not caused by vascular compression.
Like Gamma Knife treatment, radiofrequency lesioning does not treat the root cause of trigeminal neuralgia, but instead damages the trigeminal nerve to stop the transmission of pain signals. In the procedure, an electrode inserted through the cheek is used to heat the nerve and cause selective damage to stop pain signals from traveling to the brain.
The treatment provides immediate pain relief in up to 90 percent of patients. However, it does cause more facial numbness than the other procedures, and 50 percent of patients will experience pain recurrence within five years post-surgery. If necessary, the procedure can be repeated.
Radiofrequency lesioning is less invasive, less risky and requires less time in the hospital than MVD. However, it also carries a greater risk of minor to severe post-surgical numbness, which can often be permanent, in addition to the higher rate of pain recurrence. This procedure also carries the rare general surgical risks of infection and excessive bleeding, as well as excessive nerve injury, corneal numbness, anesthesia dolorosa and intracranial hemorrhage.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Treatments we specialize in
-
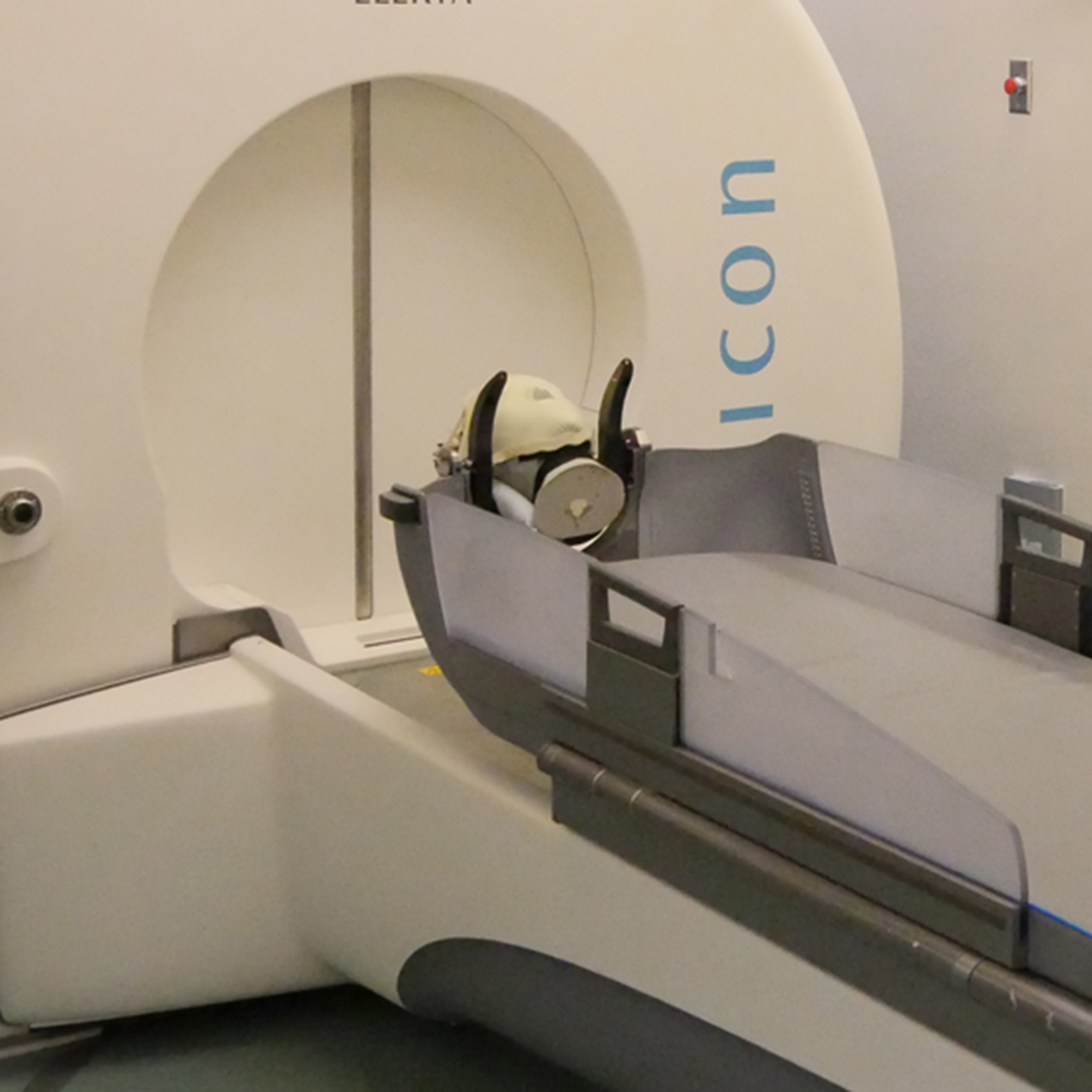
Gamma Knife
An advanced radiation procedure used to treat neurological conditions including tumors, epilepsy, trigeminal neuralgia and arteriovenous malformations.
Learn more -

Microvascular Decompression
This surgery can provide long-lasting relief for the pain of facial neuralgia by creating a buffer between a compressed nerve and the vein or artery affecting it.
Learn more -
Radiofrequency Ablation
The non-surgical procedure uses radiofrequency waves to selectively damage certain nerves, with the goal of interrupting pain signals to the brain.
Learn more





