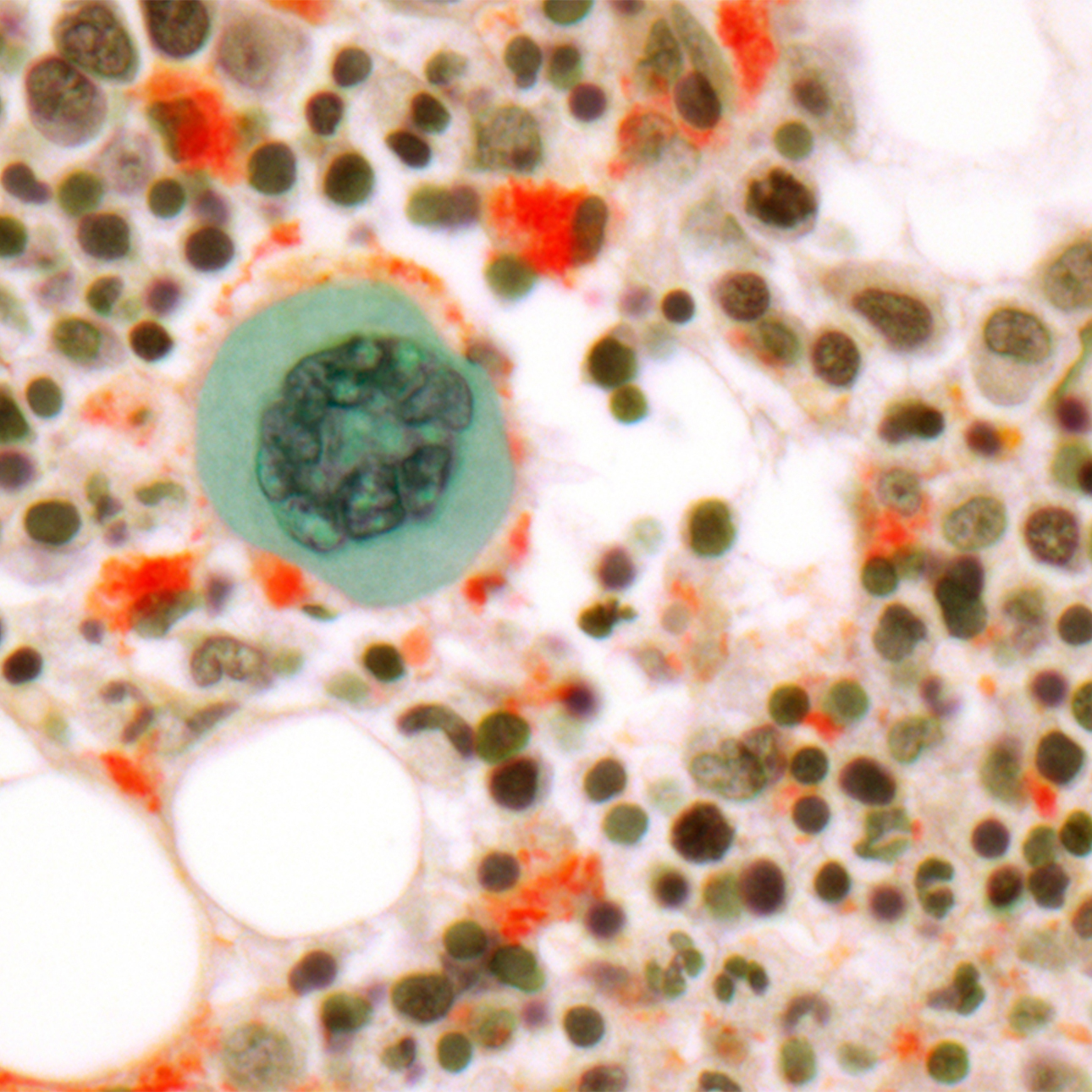
Myelodysplastic Syndromes
Treatments
The only known cure for MDS is allogeneic blood and marrow transplantation (BMT). Due to the older age of MDS patients and the intensity of allogeneic BMT, however, this treatment often isn't appropriate for MDS patients.
Allogeneic BMT achieves a cure through a combination of high-dose chemotherapy just before the transplant and an attack of the donor's immune cells against the patient's MDS cells, known as graft-versus-leukemia effect.
If allogeneic BMT is not appropriate for a patient, treatment is geared toward relieving symptoms, reducing the need for transfusions, deferring conversion to acute myeloid leukemia, and improving the quality and length of life. It does not aim to achieve a cure.
The major treatment strategies are:
- Supportive care
- Epigenetic therapy
- Biologic therapy
Supportive Care
Supportive care entails transfusions of red blood cells and/or platelets, antibiotics for the prevention or treatment of infections, chelating agents to reduce the overload of iron that accompanies red blood cell transfusions, and growth factors.
There are two agents to unload iron: desferroxamine, which is given subcutaneously up to 12 hours daily, and deseferox (Exjade), which is given orally.
The red blood cell growth factors epogen (Procrit) and darbepoetic (Aranesp) do not work well to increase red blood cell production in MDS.
The white cell growth factors filgrastim (Neupogen), pegfligrastim (Neulasta) and sargramostim (Leukine) work well to increase white cell numbers and function, helping fight or prevent infection.
Epigenetic Therapy
Epigenetic therapy consists of the intravenous or subcutaneous administration of 5-azacitidine (Vidaza) or decitabine (Dacogen). These agents turn on tumor suppression genes that are silenced in MDS.
Tumor suppressor genes make proteins that normally prevent the emergence of cancer. In MDS, tumor suppressor genes are often silenced by the addition of chemicals called "methyl groups" to the DNA backbone (an epigenetic modification). Decitabine and 5-azacitidine prevent the addition of these methyl groups and reawaken the tumor expression genes, forcing MDS cells into the background.
Epigenetic therapy is slow — requiring months for a response — and requires indefinite use to remain effective. It does not cure MDS.
Biologic Therapy
Biologic therapy is currently limited to lenalidomide (Revlimid). Through unknown mechanisms, lenalidomide improves red blood cell production in certain patients with MDS, but at the expense of lowering white blood cells and platelets.
In MDS patients missing the long arm of chromosome 5 — the "5q minus syndrome" — lenalidomide eliminates the need for red blood cell transfusions two-thirds of the time. If the main goal is to improve red blood cell production, lenalidomide is likely to be a good treatment choice.
Stem Cell Transplantation
The only know cure for MDS is an allogeneic stem cell transplant, also called a bone marrow transplant. At UCSF, there are five different allogeneic transplantation protocols available for patients with MDS. Some are only available to younger patients (those under 55), but others are available to patients up to age 70 or even 75. These experimental protocols are aimed at evaluating the safety and effectiveness of allogeneic transplantation in older patients with MDS.
With allogeneic transplantation, it is expected that 20 percent to 30 percent of patients will die early of treatment-related complications, but that a minority of patients will be cured. Results seem to be better when the transplant is performed at an earlier stage of MDS and before the disease progresses to acute myeloid leukemia. Transplantation is being investigated in patients who have a related donor as well as with donors found through the National Marrow Donor Program (NMDP).
Another option is an autologous stem cell transplant, in which patients donate their own stem cells for transplantation. Some results suggest that a small percentage of patients — perhaps up to 30 percent — may benefit from high-dose chemotherapy and re-infusion of their own stem cells.The advantage of autologous transplantation is that it does not require a donor. The disadvantage is that abnormal stem cells may be re-infused and cause MDS to develop again after the transplantation procedure.
Investigational Therapies
UCSF is dedicated to using investigational therapies and clinical research trials to improve outcomes for patients with MDS.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Treatments we specialize in
-
Allogeneic Transplant
In a procedure similar to a simple blood transfusion, the patient receives bone marrow or stem cells from a tissue-matched donor.
Learn more -

Autologous Transplant
Stem cells collected from the blood before chemotherapy or radiation are returned to the patient's body using a process similar to a blood transfusion.
Learn more





















