Infertility in Women
Treatment
Treating specific illnesses such as endometriosis may or may not treat the fertility problem. At least 10 percent of infertility problems are due to unknown causes and another 30 percent are due to problems in both the male and female partners.
In addition to medication and surgical infertility treatments to treat specific health conditions in men and women, a new class of treatments — called assisted reproductive technologies, or ART — has been developed. The most common ART is in vitro fertilization, or IVF, but new procedures can enhance the IVF process or address other infertility conditions. These procedures include:
- In Vitro Fertilization
- Intra-Uterine Insemination
- Ovulation Induction
- Male Treatments
In vitro fertilization (IVF)
In vitro fertilization, or IVF, involves fertilization in a laboratory and then the transfer of embryos into the uterus. This procedure was first used for humans in 1977 at Bourne Hall in Cambridge, England, and tens of thousands of babies have been delivered worldwide as a result of IVF treatment.
Over the years, IVF procedures have become increasingly simple, safe and more successful.
To accomplish pregnancy as a result of IVF, several steps are involved:
- Step 1 Stimulation of the ovary to produce several fertilizable oocytes (eggs)
- Step 2 Retrieval of the oocytes from the ovary
- Step 3 Fertilization of the oocytes and culture of the embryos in the IVF laboratory
- Step 4 Placement of the embryos into the uterus for implantation, called embryo transfer (ET)
Some types of infertility that may be helped with IVF include:
- Absent fallopian tubes or tubal disease that can't be treated by surgery
- Endometriosis that doesn't respond to treatment
- Genetic diseases that result in miscarriage or abnormal births
- Infertility secondary to sperm antibodies
- Male infertility caused by a low sperm count, but with enough active sperm to fertilize in the laboratory
- Male infertility in which sperm must be obtained surgically
- Unexplained infertility that doesn't respond to other treatments
UCSF offers the following procedures in conjunction with IVF:
- Egg (ovum) donor program
- Embryo and semen freezing (cryopreservation)
- Pre-implantation genetic diagnosis
Assisted hatching
Assisted hatching involves mechanical or chemical thinning of the outer shell, called the zona pellucida, of the fertilized egg prior to transfer into the uterus. The technique is used to enhance the embryo's ability to hatch or break out of its protective shell and implant in the uterus.
The procedure involves measuring the thickness of the outer shell of embryos. If an embryo has not initiated the thinning process naturally, a small "window" or hole is created chemically using a dilute acidic solution on the embryo surface. The embryos are then implanted normally into the uterus.
The most extensive experience with assisted hatching has been reported from Cornell University where implantation rates are 25 percent per embryo, as compared to 18 percent per embryo with regular IVF in non-assisted cycles.
You may be a candidate for assisted hatching if you are 38 years of age or older, or if you have previously had one or more IVF cycles with failure of your embryos to implant despite otherwise good results.
Blastocyst (embryo) culturing
Blastocyst culturing is a technique to grow embryos beyond the third day of culture. Typically, we transfer embryos into the uterus about three days after the egg retrieval, which is several days earlier than would occur in nature. On the third day, embryos generally are between six to eight cells. We now have the ability to keep the embryos two additional days in a culturing material before implanting in the uterus. During this additional culture period, the embryos continue to grow to become "blastocysts."
The natural process of embryo development begins with fertilization of the egg in the outer part of the fallopian tube. As the newly formed embryo develops, it moves slowly toward the uterine cavity where it will ultimately implant. This process takes about six to seven days. When the embryo reaches the "blastocyst" stage, it is ready to implant.
In certain patients, blastocyst culturing allows optimal selection of embryos for transfer and an increased implant rate. However, this technology may not necessarily increase your chance for pregnancy. The main advantage is that fewer embryos may be transferred to eliminate the possibility of triplet and quadruplet pregnancies, while maintaining a high pregnancy rate.
Embryo co-culturing
Embryo co-culturing was initiated in the IVF lab at UCSF Medical Center in 1999 to improve the quality of embryos prior to transfer into the womb. This technique has been used since 1996 in other centers. It involves using a buffalo rat liver cell line to secrete nutritional products that help growing embryos improve their chances for survival. This technique is only recommended to patients who have had unsuccessful IVF cycles with poor embryo quality.
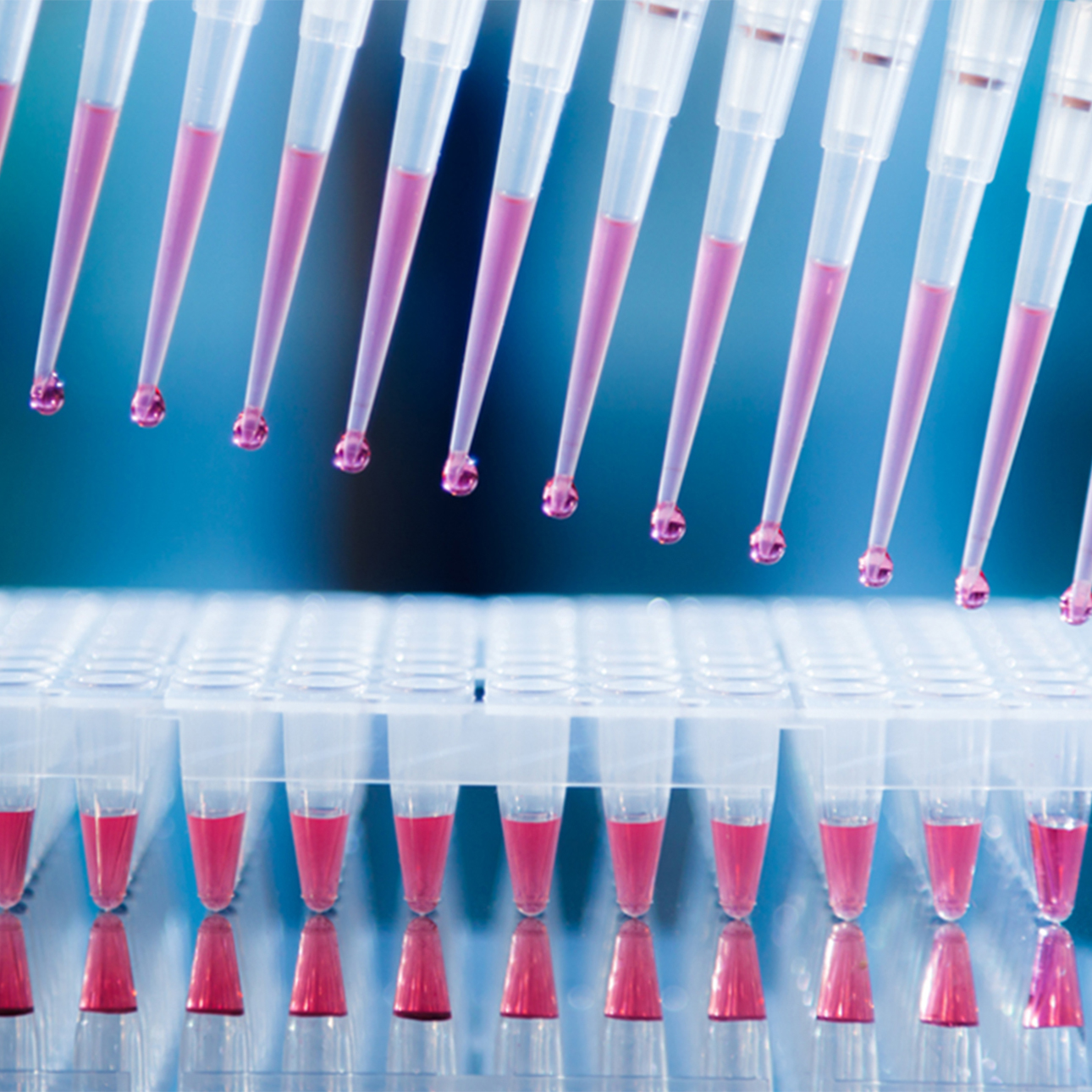
Intracytoplasmic sperm injection (ICSI)
Intracytoplasmic sperm injection, or ICSI, is the direct microinjection of a single sperm into a single egg to achieve fertilization. It was originally developed in 1992 to assist fertilization in couples with severe male factor infertility or couples who failed to fertilize in a previous IVF attempt.
The procedure overcomes many barriers to fertilization and allows couples with little hope of pregnancy to obtain fertilized embryos. The procedure was first used at UCSF Medical Center in 1994 and the first successful birth with ICSI assistance was in February 1995. UCSF Medical Center was the first San Francisco Bay Area program to achieve a pregnancy and birth with this procedure.
The technique involves very precise maneuvers to pick a single live sperm and inject it directly into the center of a human egg. The procedure requires that the female partner undergo ovarian stimulation with fertility medications so several mature eggs develop. These eggs are suctioned through the vagina, using vaginal ultrasound, and incubated under precise conditions in the embryology lab.
The semen sample is prepared by spinning the sperm cells through a special medium. This solution separates live sperm from debris and most of the dead sperm. The specialist picks up the single live sperm in a glass needle and injects it directly into the egg.
The current fertilization rate of eggs injected is 70 to 80 percent, and pregnancy rates are comparable to those seen with IVF in couples with no male factor infertility.
Please read FAQ: Intracytoplasmic Sperm Injection (ICSI) for more information about this procedure.
Intra-uterine insemination (IUI)
Intra-uterine insemination (IUI), also known as artificial insemination, is the process of preparing and delivering sperm so that a highly concentrated amount of active motile sperm is placed directly through the cervix into the uterus. The current IUI pregnancy rate per treatment at UCSF Medical Center is 14 to 15 percent. It can be performed with or without fertility drugs for the female patient.
The pregnancy rate is double that from using timed intercourse. IUI is commonly performed as a low-tech, cost-effective approach to enhancing fertility.
Please read Intra-Uterine Insemination for more information about this procedure.
Ovulation induction
Historically, oral drugs containing hormones were designed to induce ovulation in women with irregular menstrual cycles who didn't ovulate. The goal was to stimulate the body to produce and release an egg ready to be fertilized.
Later, injected hormones were developed to increase the number of eggs reaching maturity in a single cycle, increasing chances for conception. These drugs increase the risk of multiple conceptions, are more expensive, require more time and may cause ovarian over stimulation.
In the mid-90s, oral drugs were used in women with regular menstrual cycles who ovulate but who have "unexplained infertility." The drugs may treat subtle unidentified defects in ovulation and induce the maturity of two to three eggs, instead of just one, to improve both the quality and quantity of ovulation and enhance pregnancy rates.
Ovulation induction is always combined with intrauterine insemination, and it should only be considered after a complete and thorough evaluation. All underlying hormonal disorders such as thyroid dysfunction should be treated prior to resorting to using fertility drugs.
The following common fertility drugs are used for ovulation induction:
- Clomiphene Citrate — Seraphene and Clomid
- Human Menopausal Gonadotropin (hMG) — LH/FSH (Pergonal, Humegon, Repronex)
- Follicle Stimulating Hormone (FSH)
- Human Chorionic Gonadotropin (hCG) — Profasi or Pregnyl
- Leuprolide (Lupron) and Synthetic Gonadotropin (FSH/LH) Inhibitor
Please read Ovulation Induction to learn more about these drugs.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Treatments we specialize in
-

Cryopreservation
Embryos are stored at low temperatures and can be thawed later for more opportunities for conception.
Learn more -

Donor Sperm Insemination
Donor sperm can be used with in vitro fertilization (IVF) or intrauterine insemination (IUI).
Learn more -

Intrauterine Insemination (IUI)
The procedure delivers a highly concentrated amount of sperm directly into the uterus to enhance fertility.
Learn more -

In Vitro Fertilization (IVF)
Procedures to achieve IVF pregnancy have become increasingly simpler, safer and more successful than in the past.
Learn more -
Pre-Implantation Genetic Diagnosis
The laboratory procedure is combined with in vitro fertilization to reduce the risk of passing along inherited conditions.
Learn more



















