Advances in the treatment of cancer and improvements in supportive care over the past 10 years have improved the results and tolerability of stem cell transplants. However, a stem cell transplant remains an involved and potentially dangerous procedure. For autologous transplantation, the patient receives his or her own bone marrow or stem cells that were collected and frozen before admission for high-dose chemotherapy or radiation.
Autologous Transplant
Preparation
Pre-Transplant Evaluation
A stem cell transplant specialist will begin the evaluation by reviewing your medical record and history, performing a physical exam and discussing the procedure with you. If your doctor decides that you are a candidate for an autologous stem cell transplant, he or she will recommend a treatment plan.
Preadmission Tests
Before being admitted to the hospital, you will have several days of laboratory and other diagnostic tests to determine if you have normal function of the heart, lungs, kidney and liver and that you do not have an undiagnosed infection. Most of these tests will be done as an outpatient before you are admitted to the hospital, but others may need to be completed after you are admitted for treatment. These tests may include:
- Blood tests
- Urine collection
- Bone marrow aspiration and biopsy
- Chest X-ray
- Pulmonary function tests (PFTs)
- Computed tomography (CT) scan
- Electrocardiogram (EKG or ECG)
- Cardiac scan or echocardiogram
- Sinus X-rays
- Lumbar puncture
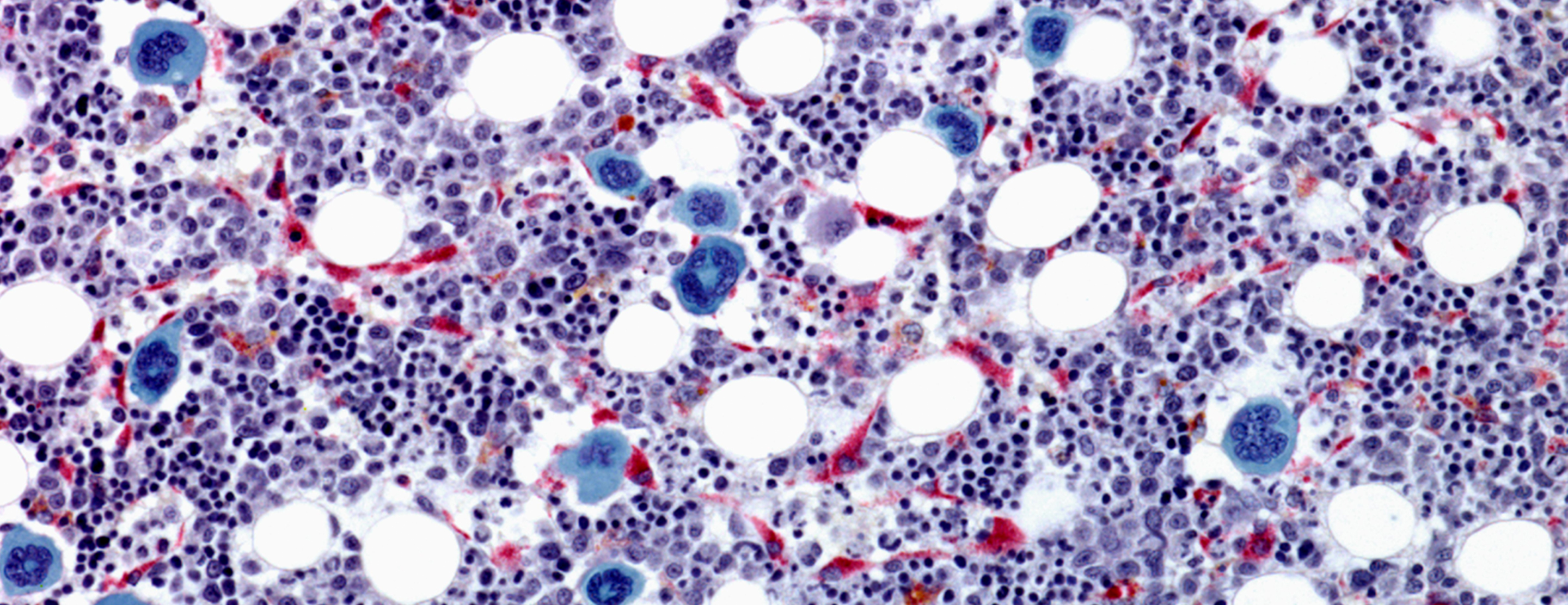
Stem Cell Collection
Stem cells are found predominantly in the bone marrow but can be stimulated to travel out into the blood. When the stem cells are collected from the hip bone via many bone marrow aspirations, which are usually performed in the operating room, the transplant procedure is called a bone marrow transplant. This is very rarely done these days. When the stem cells are collected from the blood after stimulating the stem cells with a hormone called G-CSF, or a novel agent called prelixafor, the transplant is called a peripheral blood stem cell transplant. Currently, most transplant procedures involve collecting stem cells from the peripheral blood.
When bone marrow or blood stem cells are infused into the patient, they are administered through an intravenous catheter (IV) or central venous catheter, just like a blood transfusion. The stem cells are not administered directly back into the bone, but travel to the bones from the blood stream.
For more information, visit the Pre-Transplant Evaluation and In the Hospital sections of the Autologous Transplant Guide.
Procedure
High Dose Chemotherapy
Chemotherapy begins soon after you are admitted to the hospital, after stem cell collection. Your doctor will discuss all of the drugs you will receive and their side effects. Your nurse practitioner, inpatient nurse and pharmacist also will be available to answer questions. In addition, you may receive written information on these drugs in a consent form.
Some precautions are taken to minimize side effects from these drugs. For example, when receiving some types of chemotherapy, patients must shower thoroughly twice a day to remove the drug that is excreted through the skin — this is done to help prevent or minimize chemotherapy burns. The inpatient nurse will go over any special precautions that you may need to take. Your doctor may also discuss medication (palifermin) to prevent some transplant-related complications prior to admission.
Total Body Irradiation
Some patients receive total body irradiation (TBI) in addition to chemotherapy. This radiation therapy is intended to destroy remaining cancer cells and further suppress the immune system.
TBI treatments are given in the radiotherapy department, usually over a period of three to four days. The treatment itself is painless, but there may be uncomfortable side effects after treatment, such as mouth and throat sores, nausea, stomach and intestinal irritations, and skin redness. Anti-nausea medication is usually given before each treatment to reduce nausea. You may receive additional medication (palifermin) to prevent mouth sores.
The Transplant Procedure
The transplant will occur one to three days after your last chemotherapy dose or anytime after your last radiation dose. The day of transplantation is referred to as Day 0. The days before the transplant are counted as minus days and the days after the transplant are plus days.
The procedure is similar to a simple blood transfusion and will be done in your hospital room. You may have a family member in the room with you if you wish. The actual procedure will take about 45 minutes, depending on the volume of stem cells. If you are receiving bone marrow, the infusion may take several hours. The blood stem cells will be infused through your central venous catheter.
Your nurse will check your blood pressure, temperature, breathing and pulse, and will watch for any side effects. Usually there are no side effects, but occasionally patients may experience a funny taste in the mouth, chills, flushing of the face, nausea and vomiting, headache, and changes in blood pressure and breathing.
Waiting for Engraftment
The new bone marrow does not recover immediately after it has been transplanted. The stem cells of the transplanted marrow will travel to the bones, reseed the marrow space and go through a growth process before the mature cells are released from the bone marrow into the blood stream. It will take eight to 14 days from the day of transplantation for your marrow to start producing white blood cells, red blood cells and platelets.
Engraftment is the term used to describe when your new marrow begins to function and produce cells. While awaiting engraftment, no mature cells leave the marrow and enter the blood stream. Your blood counts will show very low values and you will require careful monitoring by the health care team. The goal is to support you with red blood cell and platelet transfusion until you are producing cells again.
For more information, visit the Blood Counts and Transfusions section of the Autologous Transplant Guide.
Recovery
Delayed Side Effects
The body feels the effects of the chemotherapy or radiation about a week after transplantation. When the blood counts are low, you feel like you have the flu and may not want to do much. This will last for about two weeks and will decrease as your blood counts improve. You may notice a number of other symptoms as well, including:
- Loss of appetite
- Nausea and vomiting
- Changes in vision
- Mouth and throat soreness
- Diarrhea
- Difficulty sleeping and fatigue
- Infection
- Hair loss
- Skin reactions
- Graft-versus-host disease
Find detailed information about these side effects in the Treatment section of the Autologous Transplant Guide.
Preparing to Leave the Hospital
When your neutrophil count is over 1,000, your team will start talking to you about discharge. You will need to be sure that arrangements have been made for someone to stay with you after you are discharged, to assist you with daily needs and to be available for clinic visit transportation. You or a family member will learn how to care for your catheter.
To be discharged, you will need to be:
- Walking
- Eating at least 1,000 calories daily
- Drinking at least one quart of fluid daily
- Free of active medical problems
- Without a fever
- Off intravenous medications and taking your pills without problems
- Show that you can care for your intravenous catheter if it is needed after discharge
The case manager will assist with arrangements for home care. The nurse practitioner will go over your discharge and outpatient instructions and the pharmacist will review your medications with you.
Routine Outpatient Visits
Your BMT doctor and nurse practitioner will follow you closely after your transplantation. You will have blood work done and, if necessary, will receive intravenous medications or fluids.
Keeping Healthy
Your risk of infection will remain higher than normal for at least three months after autologous BMT, even though your body is again producing white blood cells. The highest risk is within the first month of leaving the hospital; during this period you should spend most of your time at home and away from people, which is called house arrest. You will be instructed on how to help prevent infection, including washing your hands, avoiding large crowds and refraining from smoking.
Get more information about taking care of yourself after a BMT in the Outpatient Care section of the Autologous Transplant Guide.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.